Back to 2025 Abstracts
The Cost of Complications: How Socioeconomic Status Shapes Radical Cystectomy Outcomes
Adam Cole, MD1, Connor Pelletier, BS
1, Emilie Platteter, BS
2, Randie White, MD
1, Evelyn James, MPH
1, Joshua Linscott, MD, PhD
3, Jeffrey Howard, MD, PhD
1, Stephen Ryan, MD
1, Matthew Hayn, MD
1, Jesse Sammon, DO
1.
1Maine Medical Center, Portland, ME, USA,
2University of New England, Portland, ME, USA,
3Moffitt Cancer Center, Tampa, FL, USA.
BACKGROUND: Radical cystectomy (RC) is a complex procedure with high postoperative complication rates. Our institution provides the most RC care in a rural state, where socioeconomic status (SES) is thought to influence surgical outcomes. We evaluated the impact of predicted SES on RC outcomes.
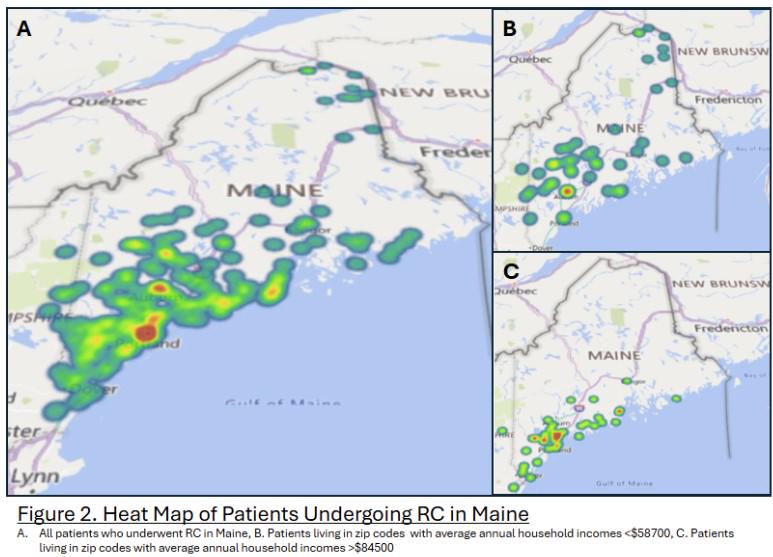
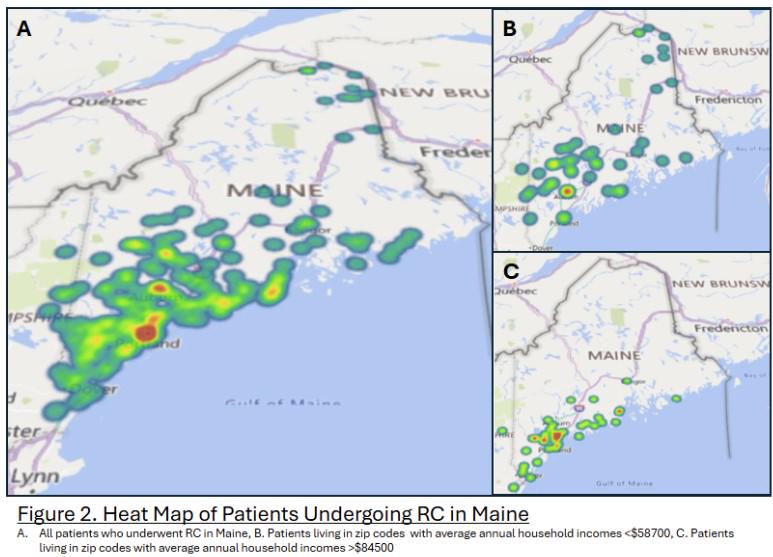
METHODS: We analyzed 331 RC patients (2015-2024) using a prospectively maintained database with complete 90 day follow up. SES was estimated from 2020 census data using average annual income and the percentage of bachelorís degree holders within a patientís ZIP code. Multivariable logistic regression assessed complications, readmissions, 90-day mortality, and length of stay.
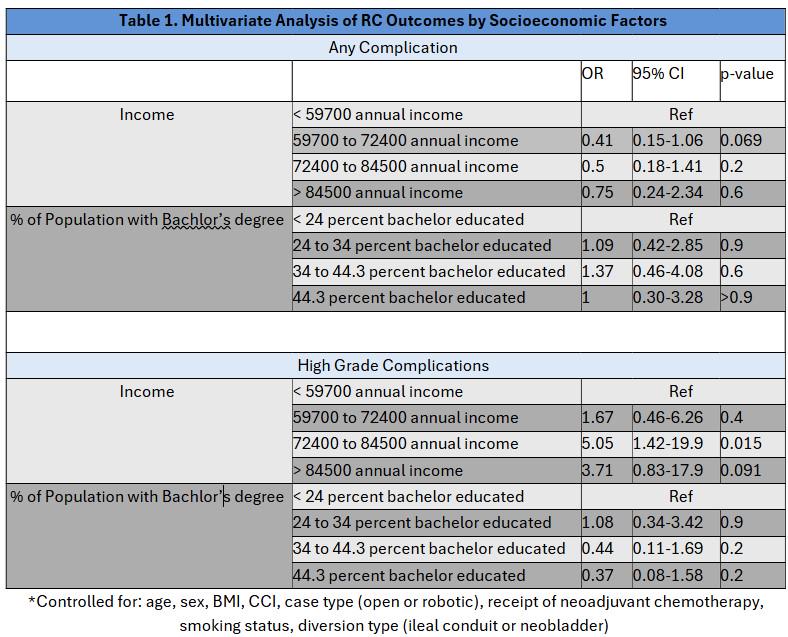
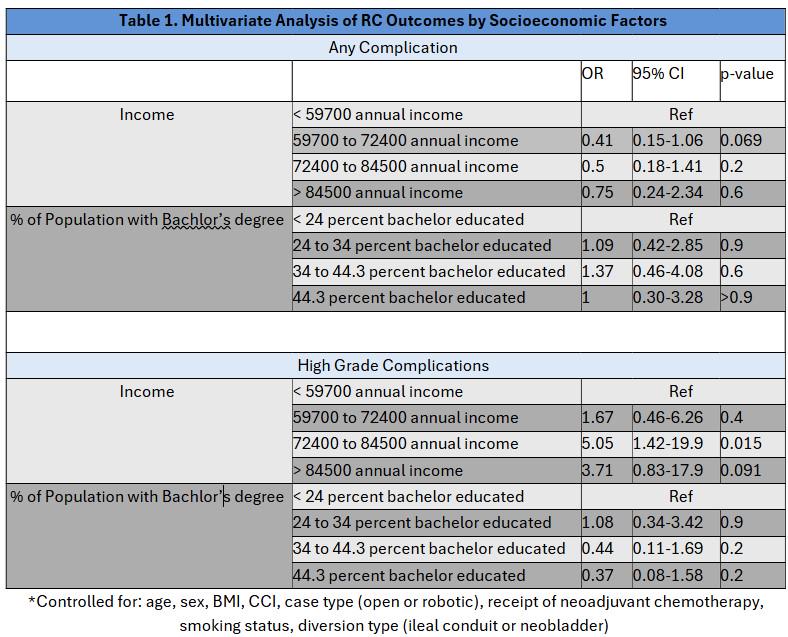
RESULTS: Patients from ZIP codes with average incomes of $59,700-$72,400 had fewer complications (OR 0.41, 95% CI 0.15-1.06, p=0.069), trending toward significance. Those from higher-income ZIP codes ($72,400-$84,500) had increased risk of high-grade complications (OR 5.05, 95% CI 1.42-19.9, p=0.015) (Table 1). Income did not predict other outcomes, and average education level was not significantly associated with complication severity, readmission, or length of stay.
CONCLUSIONS: SES inconsistently predicted RC outcomes. Patients from moderate-income areas had fewer complications, while those from higher-income areas had greater risk of severe complications. Our study demonstrates that ZIP code-based SES estimates may not accurately reflect individual SES in rural states with uneven wealth distribution. Alternatively, SES may have less impact on postoperative outcomes than assumed.
Back to 2025 Abstracts