Back to 2025 Abstracts
Dynamic Prediction of Recurrence and Progression Risk in Non-Muscle Invasive Bladder Cancer Using Conditional Survival: A SEER-Medicare Analysis
Chia-Chen Chang, MS1, Agustin Perez-Londono, MD
2, Sumedh Kaul, MS
2, Aaron Fleisham, MD
2, Simon Kim, MD
3, Aria Olumi, MD
2, Peter Chang, MD, MPH
2, Andrew Wagner, MD
2, Boris Gershman, MD
2.
1Georgetown University, Washington, MA, USA,
2Beth Israel Deaconess Medical Center, Boston, MA, USA,
3University of Colorado Anschutz Medical Center, Aurora, CO, USA.
BACKGROUND: Predicting recurrence and progression risk in non-muscle invasive bladder cancer (NMIBC) is essential for counseling and risk-adapted management. However, conventional models do not account for the change in baseline risk over the time. We examined the conditional survival free of recurrence and progression among older adults with NMIBC to develop a dynamic risk prediction model.
METHODS: We identified patients aged 66-89 years with a diagnosis of Ta/Tis/T1 cN0 cM0 bladder cancer treated with TURBT from 2000-2017 in the SEER-Medicare linked database. Conditional recurrence-free (RFS) and progression-free (PFS) survival were estimated using the Kaplan-Meier method. Associations of baseline characteristics with RFS and PFS at pre-specified landmark times were evaluated using Cox proportional hazards models.
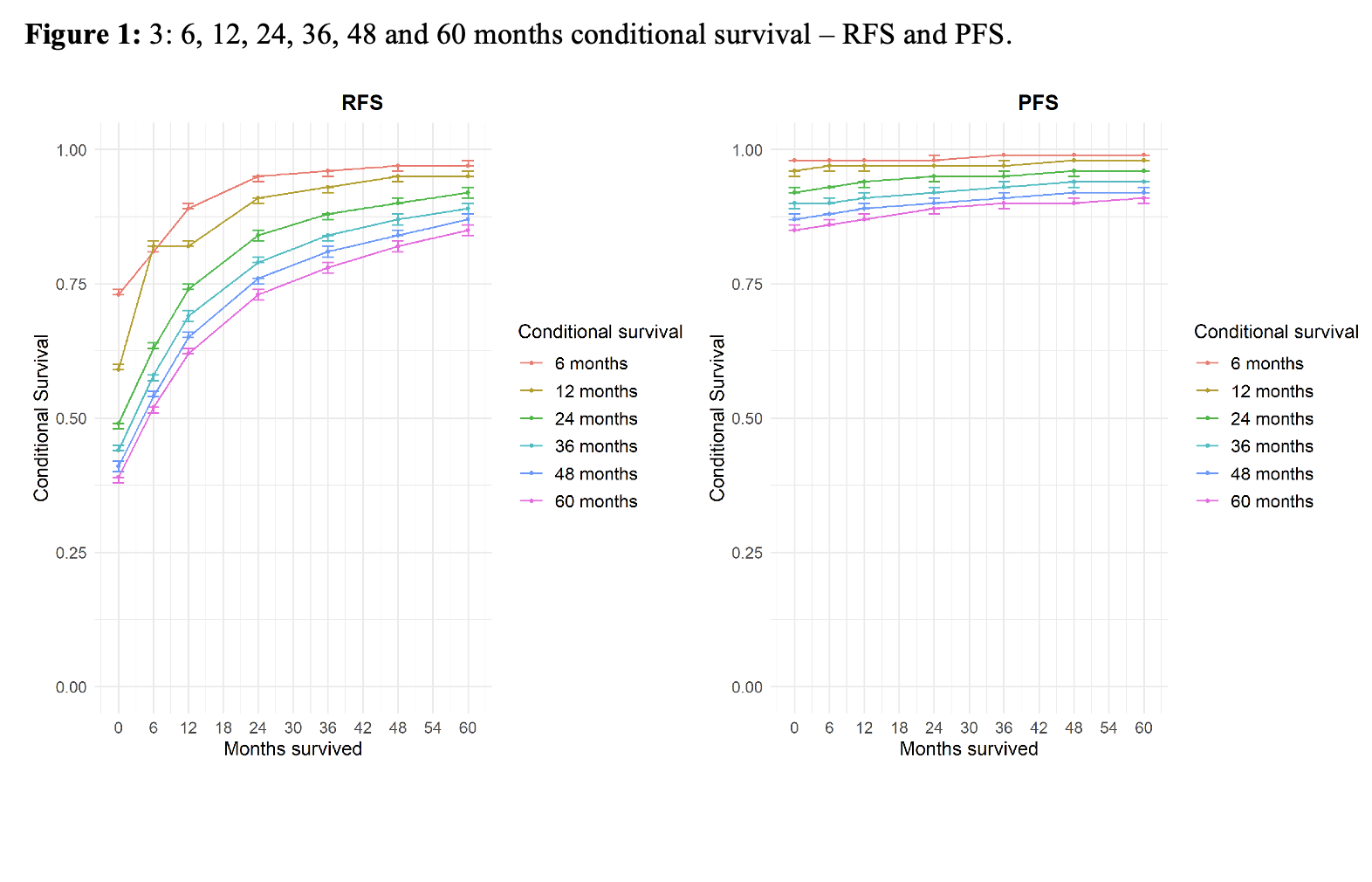
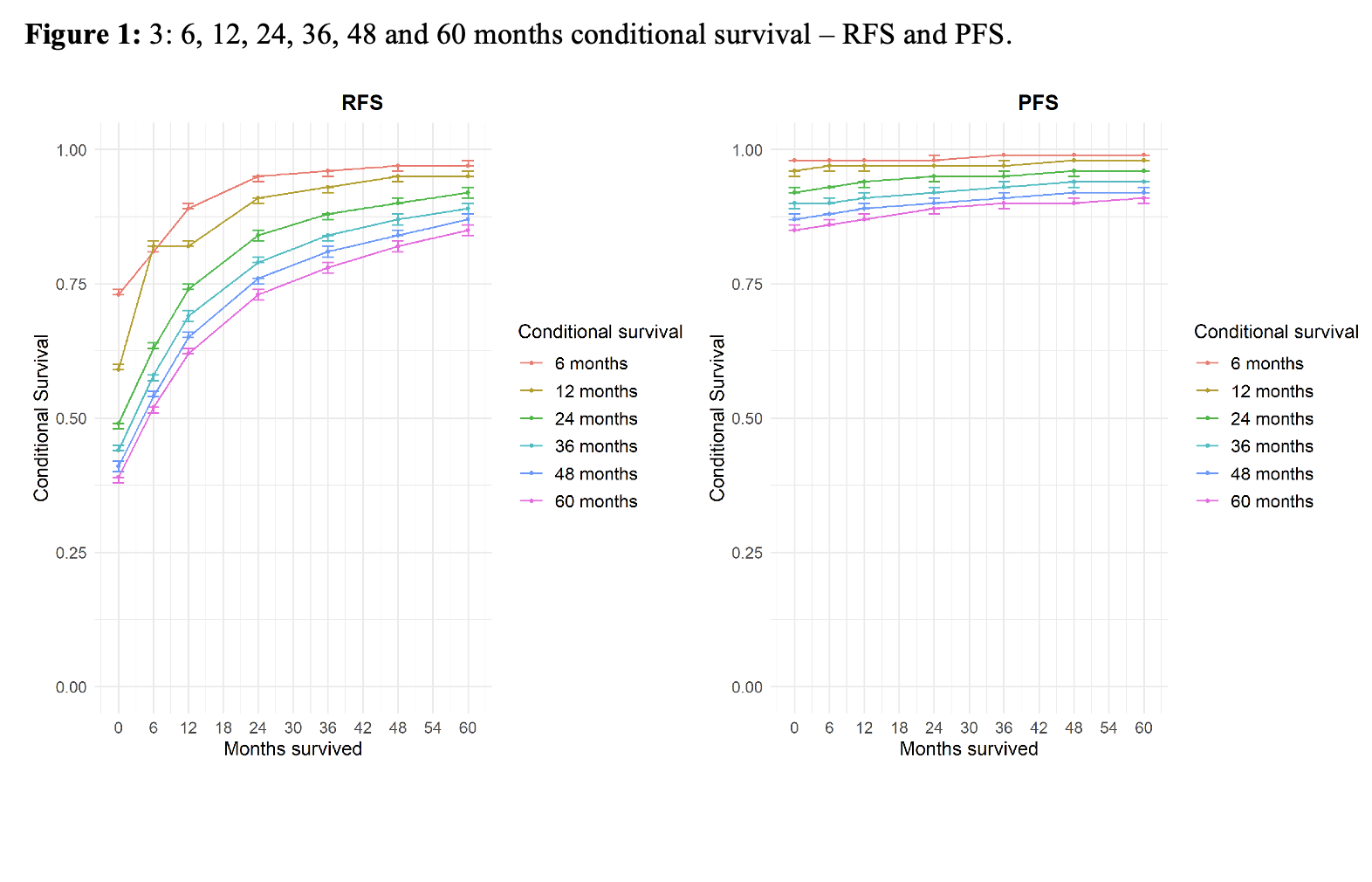
RESULTS: A total of 39,862 patients were included. Of these, 26,339 (66%) had Ta, 11,758 (29%) had T1, and 1765 (4%) had Tis disease. Median follow-up was 65 months. Baseline 60-month RFS and PFS were 0.39 and 0.85 respectively. Given a 6-, 12-, 24-, 36-, 48-, and 60-months event-free survivorship, the 60-month RFS and PFS were 0.52, 0.62, 0.73, 0.78, 0.82, 0.85 and 0.86, 0.87, 0.89, 0.90, 0.90, and 0.91 respectively
(Figure 1). Conditional RFS rapidly improved within the first 24 months, then plateaued. When stratified by T-stage, patients with T1 disease demonstrated the greatest improvement in conditional RFS. On multivariable analyses, T-stage and tumor grade were less predictive of RFS with longer landmark times.
CONCLUSIONS: Among patients with NMIBC, the risks of disease recurrence and progression decrease with longer event-free intervals. These observations are most pronounced among those at highest risk, as evidenced by tumor stage and grade. Dynamic risk prediction can improve patient counseling and risk-adapted management during follow-up.
Back to 2025 Abstracts