Back to 2025 Abstracts
Comparison of Opioid Requirements after Peripheral Nerve Block in Standard and mini Percutaneous Nephrolithotomy
OLAMIDE OLAWOYIN, MD, Ankur U. Choksi, MD, Mursal Gardezi, MD, Jinlei Li, MD, PhD, Piruz Motamedina, MD.
Yale New Haven Health, NEW HAVEN, CT, USA.
BACKGROUND: Mini percutaneous nephrolithotomy (PCNL) compared to standard-PCNL lowers peri-operative complications while maintaining comparable stone-free rate (SFR). There is limited data comparing peri-operative opioid requirements particularly when peripheral nerve blocks (PNB) is administered. We aim to assess overall opioid requirements in standard-PCNL vs. mini-PCNL after PNB.
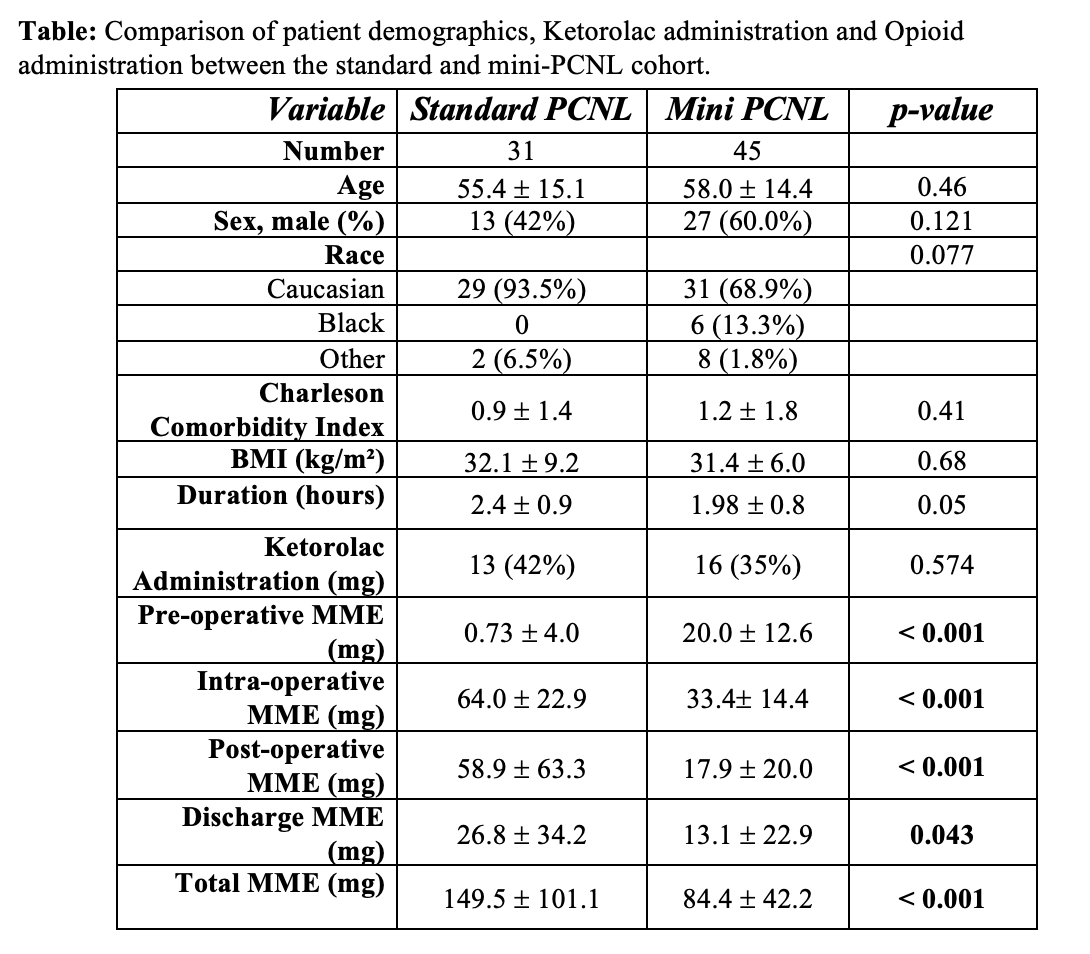
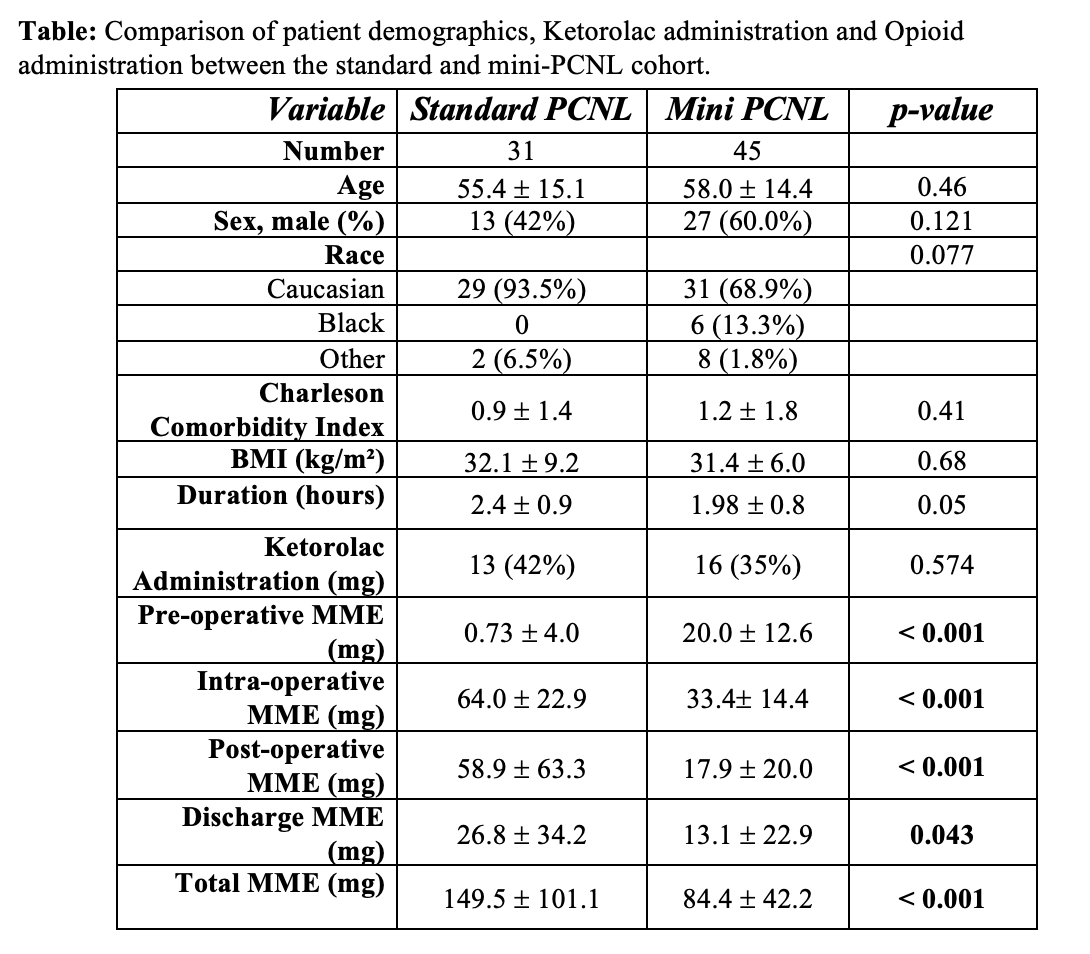
METHODS: We performed a retrospective cohort review of patients who underwent standard and mini-PCNL and received pre-operative PNB between 2021 and 2024. Patient demographics, NSAIDs and opioid administration were analyzed. Opioid requirement was measured as oral morphine milligram equivalents (MMEs) and categorized as pre-operative, intra-operative, and post-operative. Univariate analysis with Chi-squared test was performed to analyze categorical variables. Univariate analysis with two tailed t-tests was performed to analyze continuous variables.
Results: On retrospective review, 76 patients who underwent PCNL received a PNB. Standard-PCNL was performed in 31 patients and mini PCNL was performed in 45 patients. 24-french balloon dilator was used in the standard-PCNL vs. a 17.5-french dilator for mini-PCNL. There was no difference in age, sex, race, BMI and comorbidities between both groups. Operative duration was slightly longer in the standard-PCNL vs. mini-PCNL (2.4 ± 0.9 hours vs. 1.98 ± 0.8, p = 0.05). A significantly higher dosage of ketorolac was administered in those who underwent standard-PCNL compared to mini-PCNL (19.8 ± 35.8 vs. 6.7 ± 10.4, p = 0.022). Pre-operative, intra-operative and post-operative opioid requirements was significantly higher in standard-PCNL (p <0.001, <0.001 and 0.043 respectively). Total opioid requirements remained significantly higher in the standard-PCNL group after controlling for age, BMI, Charlson comorbidity index and race, and duration of surgery(p = 0.005).
Conclusion: When PNB is performed, mini-PCNL is associated with less opioid use compared to standard-PCNL.
Back to 2025 Abstracts