Back to 2025 Abstracts
Trends in Prostate MRI Adoption Before Biopsy Among Commercially Insured Patients
Shayan Smani, BS1, Rong Wang, PhD
2, Preston Sprenkle, MD
1, Cary P. Gross, MD
3, Xiaomei Ma, PhD
2, Michael Leapman, MD MHS
1.
1Department of Urology, Yale University School of Medicine, New Haven, CT, USA,
2Department of Chronic Disease Epidemiology, Yale University School of Public Health, New Haven, CT, USA,
3Department of Internal Medicine, Yale University School of Medicine, New Haven, CT, USA.
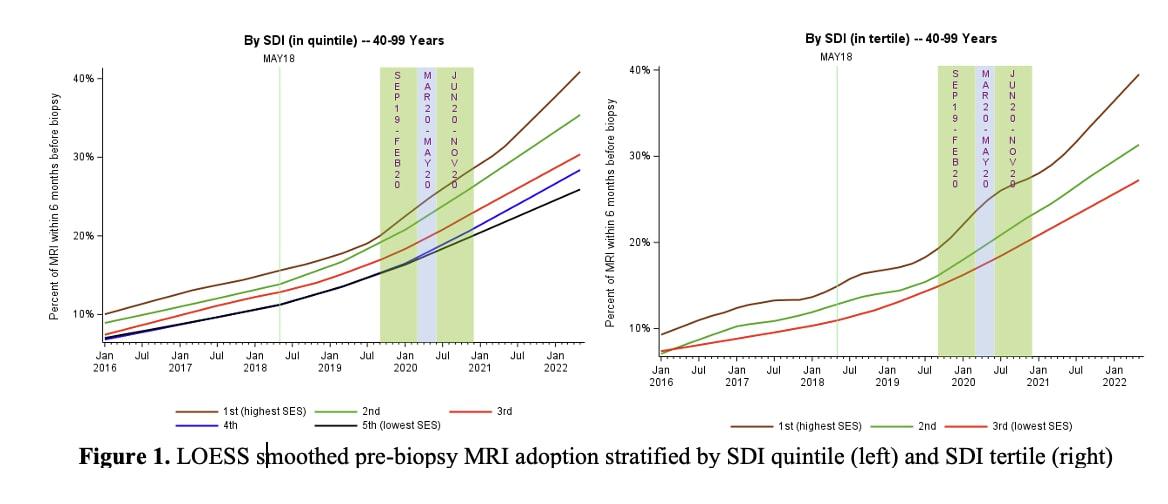
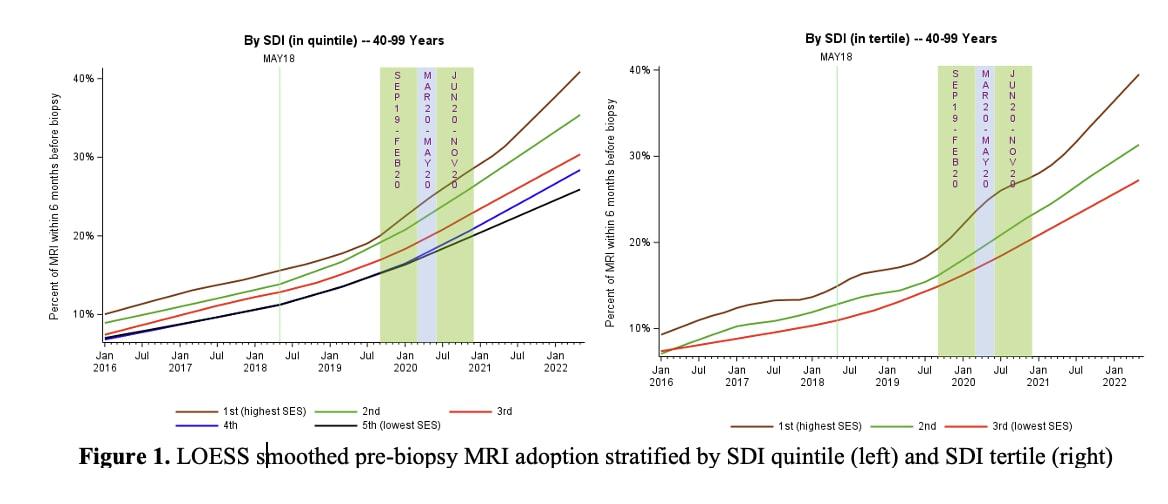
BACKGROUND: Although prostate MRI is associated with increased cancer detection and accuracy of initial prostate cancer diagnosis, national uptake in the United States has been slow and incomplete. We evaluated time trends and area-level sociodemographic factors associated with prostate MRI use prior to prostate biopsy.
METHODS: We conducted a retrospective, dynamic cohort study of Blue Cross Blue Shield insurance beneficiaries aged 40-99 to assess the use of prostate MRI before prostate biopsy. The primary objective was to evaluate the association between social deprivation index (SDI), a composite measure of area level deprivation and changes in bimonthly rates of PSA testing.
RESULTS: Among 112,567 patients undergoing prostate biopsy from 2016 to 2022, the proportion receiving pre-biopsy MRI increased from 9.45% in early 2016 to 33.19% by mid-2022 (p-trend<.01). Utilization was highest among patients aged 70-99 (19.8% overall; 35.26% in 2022) and lowest among those under 50 (16.15% overall; 31.30% in 2022). MRI use varied significantly by geography and socioeconomic status. Patients in metropolitan areas had higher utilization (35.41% in 2022) compared to non-metropolitan areas (22.50%). MRI use also differed by Social Deprivation Index (SDI), with those in the least deprived areas having significantly higher rates (39.69% in 2022) than those in the most deprived areas (26.03%, p<0.01). States such as Massachusetts, California, and Michigan saw the greatest absolute increases in utilization. Despite growth, disparities in MRI adoption persist based on socioeconomic and geographic factors.
CONCLUSIONS: While prostate MRI utilization has grown, its adoption remains uneven, underscoring disparities tied to socioeconomic and geographic factors. Efforts to expand MRI access, particularly in underserved populations, are essential to align care with clinical guidelines and improve diagnostic equity in PCa.
Back to 2025 Abstracts