Back to 2025 Abstracts
The OptilumeŽ Drug Coated Balloon for recurrent anterior urethral strictures: ROBUST III study 4-year results
Sean Elliott, MD
1,
Karl Coutinho, MD2, Kaiser Robertson, MD
3, Richard DAnna, MD
4, Kent Chevli, MD
5, Serge Carrier, MD
6, Melanie Aube-Peterkin, MD
6, Christopher H. Cantrill, MD
7, Michael J. Ehlert, MD
8, Alexis E. Te, MD
9.
1University of Minnesota, Minneapolis, MN, USA,
2Summit Medical Group, Millburn, NJ, USA,
3Chesapeake Urology, Hanover, MD, USA,
4Arkansas Urology, Little Rock, AR, USA,
5Western New York Urology Associates, Cheektowaga, NY, USA,
6McGill University Health Center, Montreal, QC, Canada,
7Urology San Antonio, San Antonio, TX, USA,
8Metro Urology, Woodbury, MN, USA,
9Weill Cornell Medicine, New York, NY, USA.
Title: The OptilumeŽ Drug Coated Balloon for recurrent anterior urethral strictures: ROBUST III study 4-year results
Introduction: The ROBUST III study is a randomized controlled trial comparing the OptilumeŽ Drug Coated Balloon (DCB) against DVIU or dilation. The OptilumeŽ Drug Coated Balloon (DCB) is a dilation balloon with a paclitaxel coating that combines mechanical dilation for immediate symptomatic relief with local drug delivery to maintain urethral patency. Outcomes after 4-year follow-up are presented here.
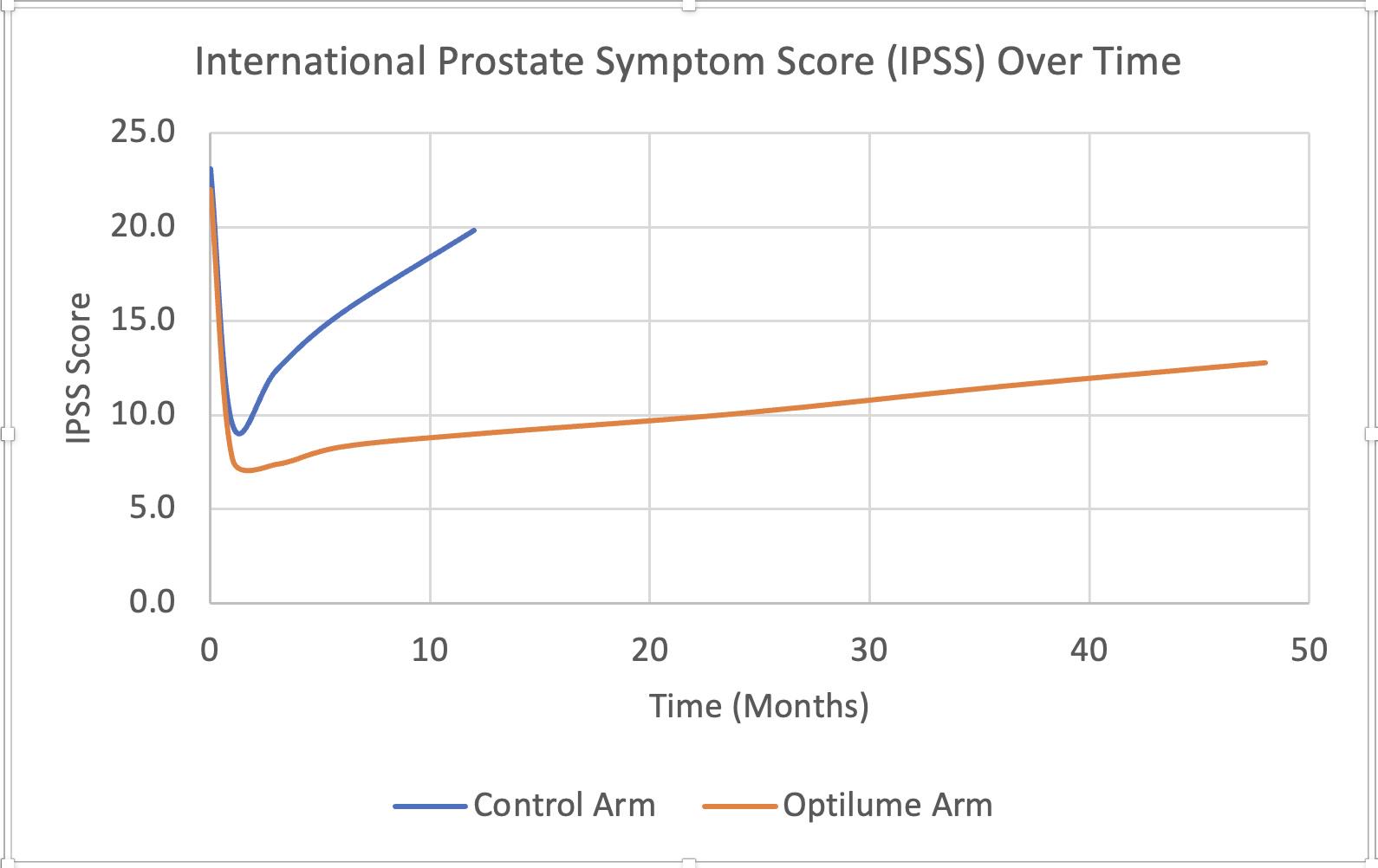
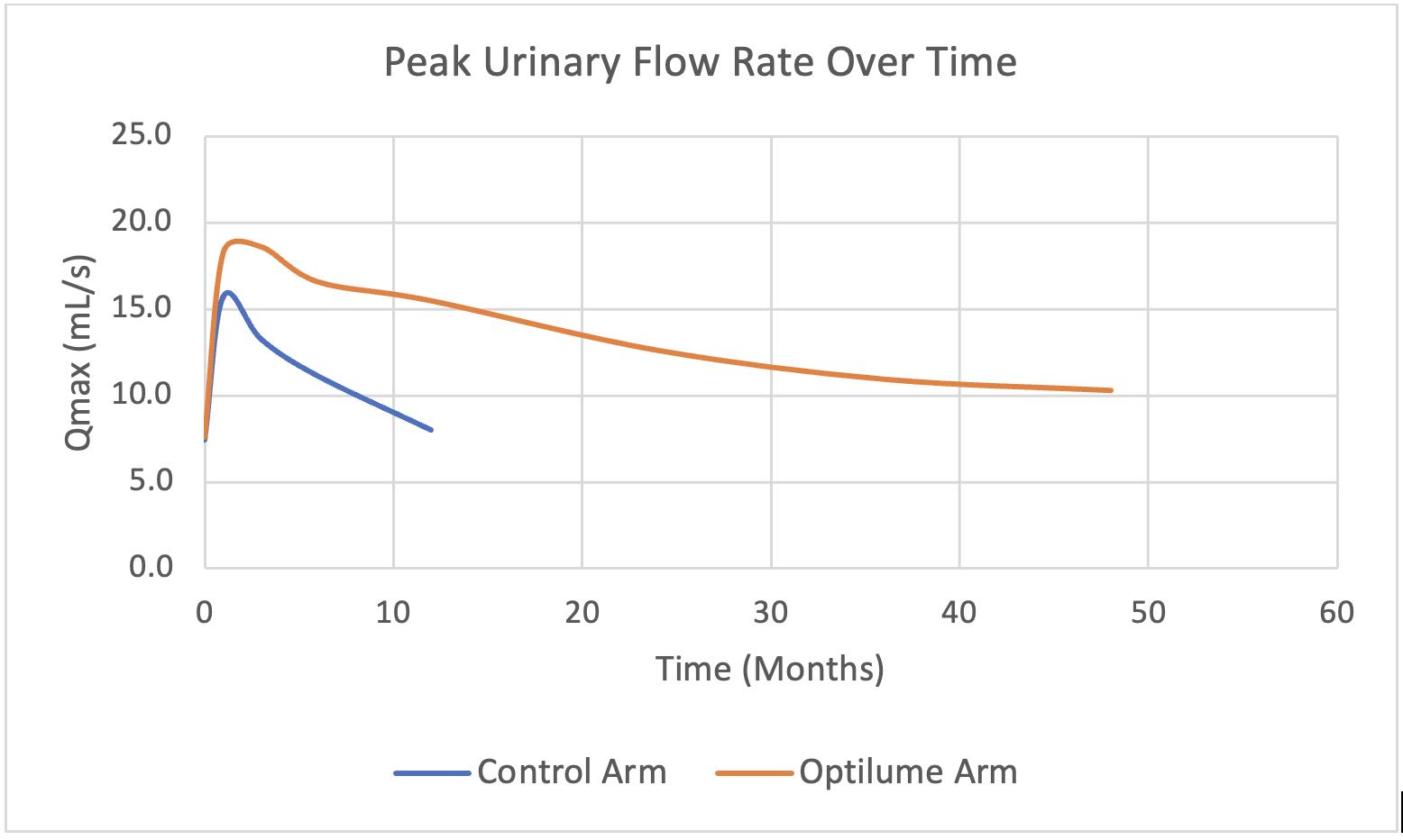
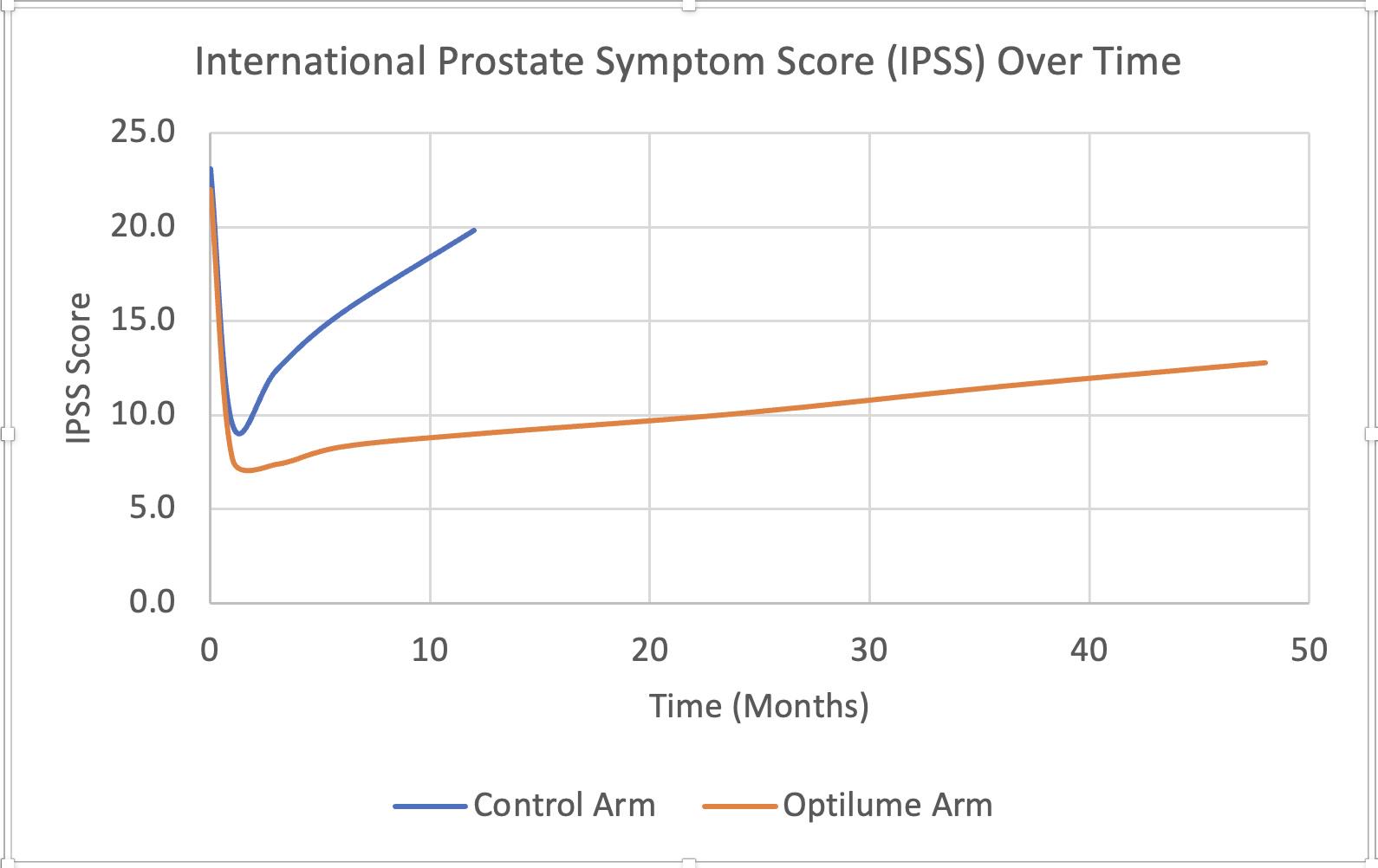
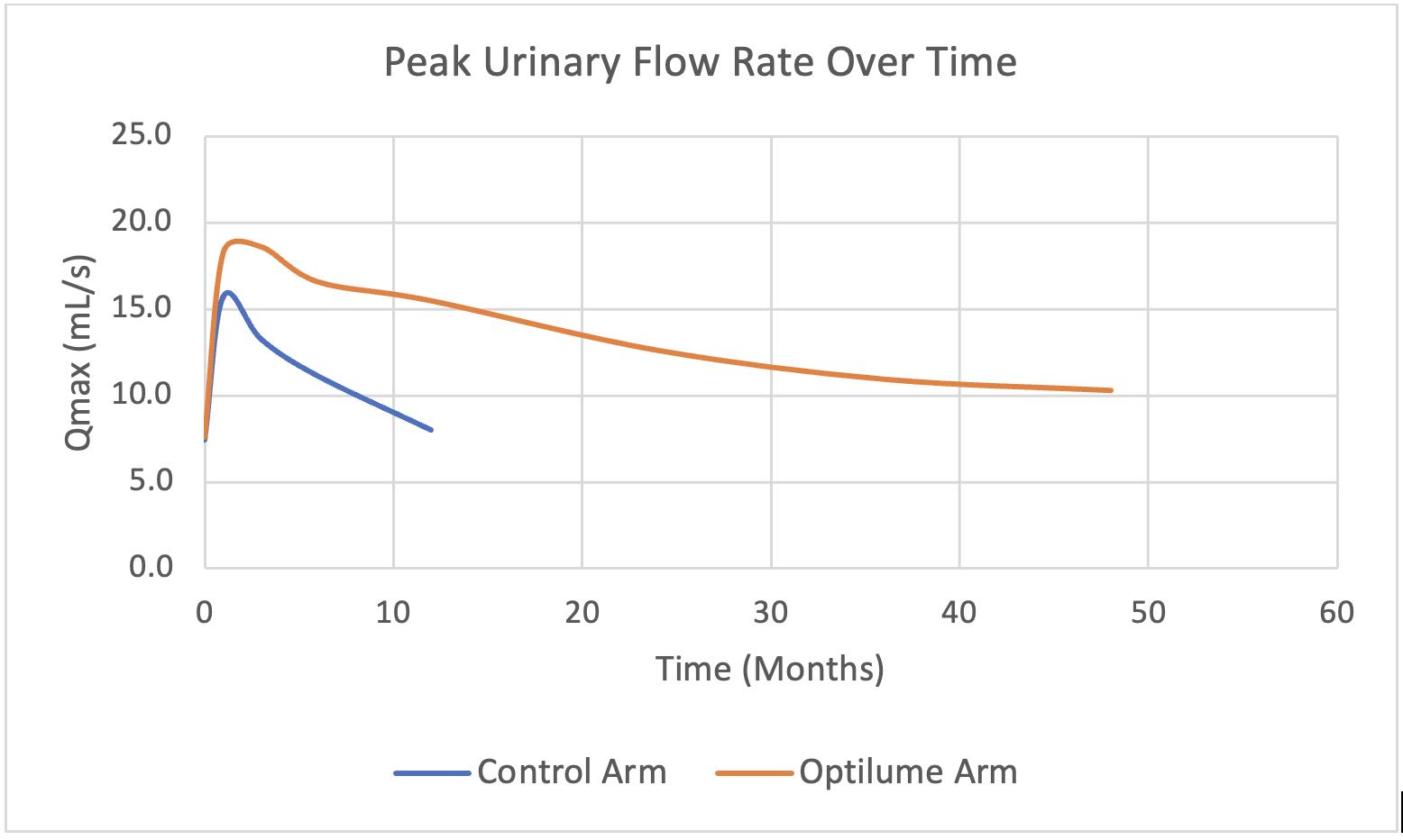
Materials & Methods: 127 subjects were randomized in a 2:1 fashion at 23 sites - 79 were treated with the DCB and 48 were treated with DVIU or dilation. Follow-up past 1 year was limited to those treated with the DCB. Eligibility criteria included adult males with anterior strictures with ≥2 prior treatments and stricture length ≤3cm. Long-term endpoints included freedom from repeat treatment, International Prostate Symptom Score (IPSS), and peak urinary flow rate (Qmax).
Results: Subjects randomized to receive the DCB had an average of 3.2 prior treatments and average stricture length of 1.6cm (46% ≥2cm), with 8/79 (10.1%) having penile strictures and 9/79 (11.4%) having prior pelvic radiation. IPSS significantly improved from 21.9 at baseline to 12.8 at 4 years. Qmax significantly improved from a baseline of 7.7 mL/sec to 10.3mL/sec at 4 years. Freedom from repeat intervention for DCB subjects was estimated to be 68%. No late-onset treatment related adverse events were observed.
Conclusions: The OptilumeŽ DCB continues to achieve significant improvements in symptoms, flow, and reintervention rates through 4 years post treatment.
Back to 2025 Abstracts