Back to 2016 Annual Meeting
Ureteroscopic Laser Endopyelotomy: A Minimally Invasive Option for Short-Segment UPJ Stricture Following Pediatric Pyeloplasty?
Paul Smith, III, MD, Katherine W. Herbst, MS, Melinda Carpenter, MS, Christina Kim, MD.
Connecticut Childrens Medical Center, Hartford, CT, USA.
Background: Dismembered pyeloplasty by open, robotic, or laparoscopic approaches is a highly effective procedure for treatment of ureteropelvic junction (UPJ) obstruction in children. Recurrent or persistent UPJ obstruction following pyeloplasty is an uncommon event, for which reoperative pyeloplasty is generally considered the gold standard treatment. We reviewed our experience with retrograde ureteroscopic laser endopyelotomy as a minimally invasive treatment for failed pediatric dismembered pyeloplasty in selected patients.
METHODS: We identified all pediatric patients undergoing retrograde ureteroscopic laser endopyelotomy for treatment of failed dismembered pyeloplasty at our institution between January 2006 and June 2015. Patient demographic, operative, radiographic, and clinical data were abstracted from the medical record. Successful endopyelotomy was defined by absence of clinical or radiographic evidence of recurrent or persistent obstruction at last follow up with a minimum duration of 12 months follow up after endopyelotomy.
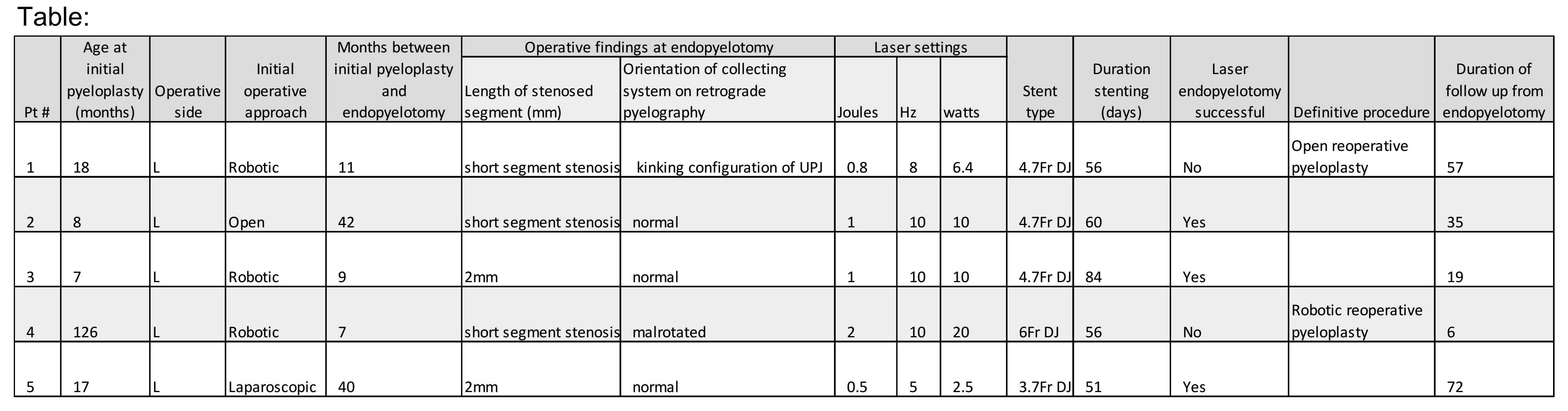
RESULTS: Five patients who underwent retrograde ureteroscopic holmium laser endopyelotomy met inclusion criteria (Table). The initial pyeloplasty was performed by an open (1), robotic (3), or laparoscopic (1) approach. The primary pyeloplasty was performed at a median age of 17 months (IQR=65). The median interval between primary pyeloplasty and laser endopyelotomy was 11 months (IQR=33). Endopyelotomy was performed by deep posteriolateral laser incision to the level of peripelvic fat followed by balloon dilation to 12Fr in all patients. An internalized ureteral stent was left in place for an average 61 days following endopyelotomy. Three patients showed no evidence of recurrent obstruction at mean follow up of 42 months. All patients with successful endoscopic treatment were found to have normal orientation of the UPJ and short segment (≤2mm) stenosis at the time of endopyelotomy. Of the patients who failed endopyelotomy, one was noted to have a malrotated kidney and the other was noted to have an abnormal insertion of the ureter into the UPJ that resulted in a kinking phenomenon. Patients who failed endoscopic management were subsequently treated with reoperative pyeloplasty.
CONCLUSIONS: Because recurrent obstruction following pediatric pyeloplasty is uncommon, the optimal management of these patients remains unclear. Advances in holmium laser and endourologic equipment have made retrograde ureteroscopic laser endopyelotomy a technically feasible option for treatment of the failed pediatric pyeloplasty. We show that retrograde ureteroscopic laser endopyelotomy may be a successful treatment option for the failed pyeloplasty in selected patients with short segment UPJ stricture and otherwise normal UPJ configuration. 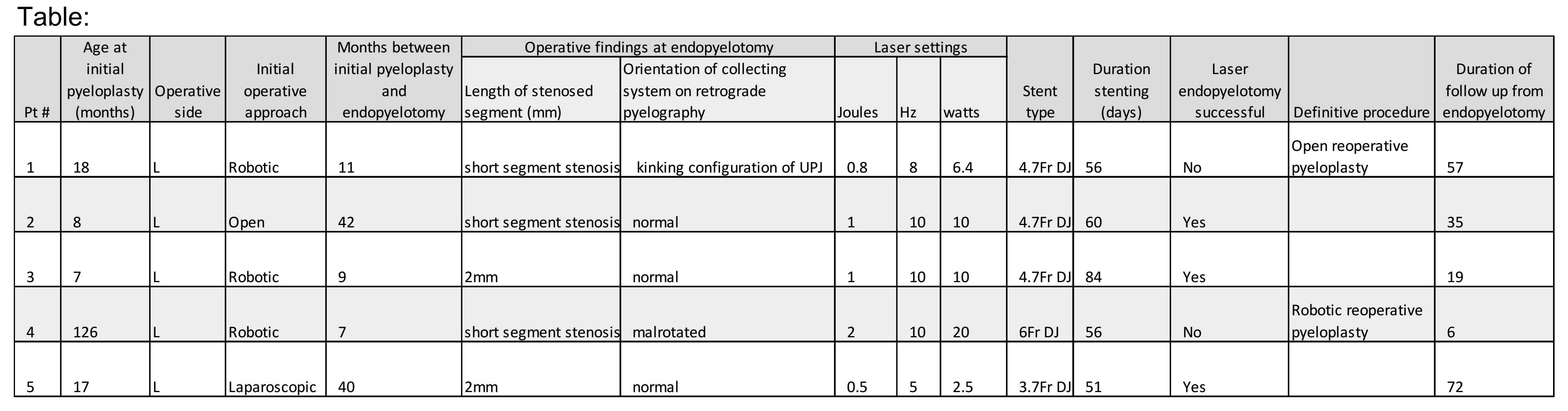
Back to 2016 Annual Meeting
|
|
|