Back to 2016 Annual Meeting
The role of patient-specific 3D prostate model based on preoperative MRI for robot-assisted laparoscopic prostatectomy
Philip J. Cheng, MD, Michael E. Zavaski, MD, Junichi Tokuda, PhD, Nobuhiko Hata, PhD, Clare M. Tempany, MD, Adam S. Kibel, MD.
Brigham and Women's Hospital, Boston, MA, USA.
Background
The goal of robot-assisted laparoscopic prostatectomy (RALP) is to completely excise the prostate cancer and gland while maximizing the postoperative erectile function by preserving the neurovascular bundles (NVB) and urinary function by preserving the external urinary sphincter (EUS). The objective of this study is to evaluate the impact of patient-specific 3D models, generated from MRI, on intraoperative decision-making.
Methods
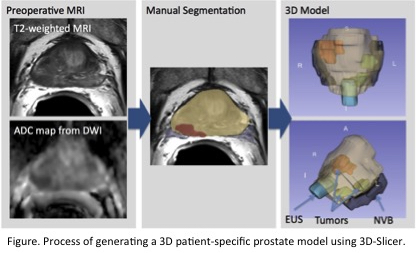
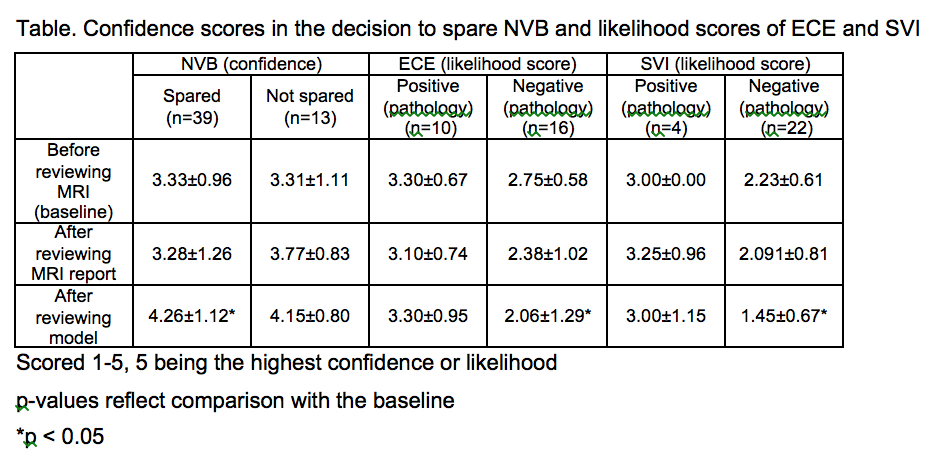
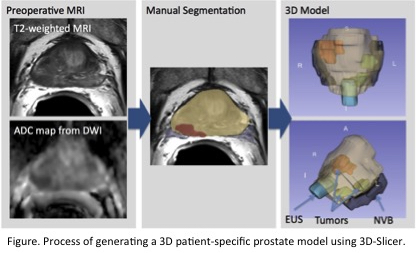
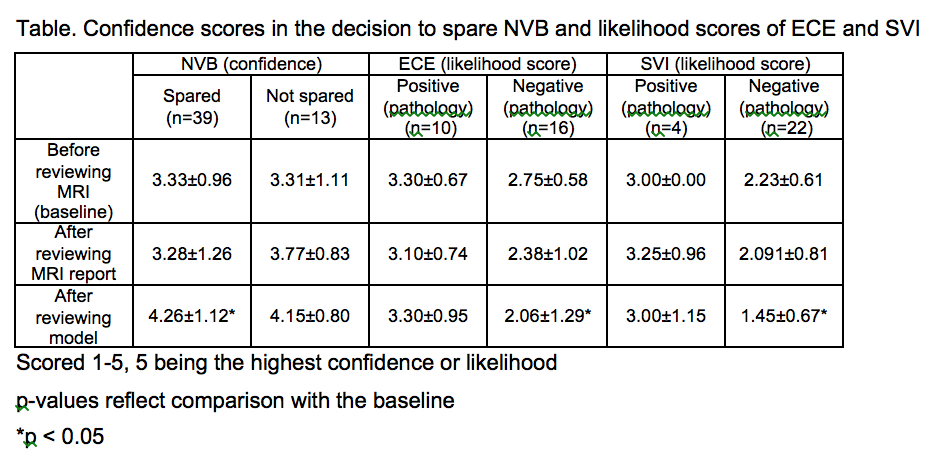
Twenty-six subjects underwent a RALP by a single surgeon and pre-operative 3 tesla MRI under IRB-approved protocol. The following structures were segmented manually using the 3D Slicer (open source software: www.3DSlicer.org) to generate the individual’s 3D prostate model (see figure): whole gland, NVBs, EUS, and all tumors. At 3 different time points, (1) before reviewing the MRI, (2) after reviewing the MRI, and (3) after reviewing the 3D model, the surgeon provided (A) decision regarding NVB sparing for each side, (B) likelihood of extracapsular extension (ECE) and (C) likelihood of seminal vesicle involvement (SVI). For (A), the surgeon also scored the confidence in his answers (1-5; 5 is highest). The decisions regarding NVB sparing were also correlated with left posterior and right posterior margins in the histopathology. Confidence scores were compared with the final decision, while (B) and (C) were compared with the histopathology.
Results
Among 52 NVBs, 39 were spared and 13 were resected. 6 were changed from non-nerve-sparing (NNS) to nerve-sparing (NS) after reviewing the 3D model. 4 of these cases had negative margins on pathology, which shows that change in management was correct in 67% of the cases. None were changed from NS to NNS. Following review of the 3D prostate model, the surgeon was more confident in sparing the NVB (p < 0.001) when compared to confidence scores before reviewing the MRI. The surgeon also reported a lower pre-operative likelihood of ECE and SVI in patients with negative pathology (p = 0.04 for ECE, p < 0.001 for SVI).
Conclusions
The confidence in the decision to spare the NVB increased significantly after reviewing the 3D model. Review of the 3D model provided better prediction of negative ECE and SVI. The 3D model can help surgeons make decisions regarding NVB sparing.
Acknowledgements This work is supported in part by R01CA111288, 2P41 EB015898-11, P01CA067165, U01CA151261, U54EB005149 from NIH, and Center for Integration of Medicine and Innovative Technology (CIMIT11-325).
Back to 2016 Annual Meeting
|
|
|