|
Back to 2015 Joint Annual Meeting
To Perc or to Scope: Is a Urologic Approach to Ureteroenteric Strictures Superior?
Nathan M Shaw, Rebecca Zee, Jennifer Lobo, Tracey L Krupski
University of Virginia, Charlottesville, VA
Introduction: Ureteroenteric stricture occurs in up to 15% of patients after cystectomy with urinary diversion. First-line management is typically percutaneous nephrostomy (PCN) drainage. We sought to compare costs and timeline for treatment of a urologic approach with flexible endoscopy and retrograde ureteral stent placement.
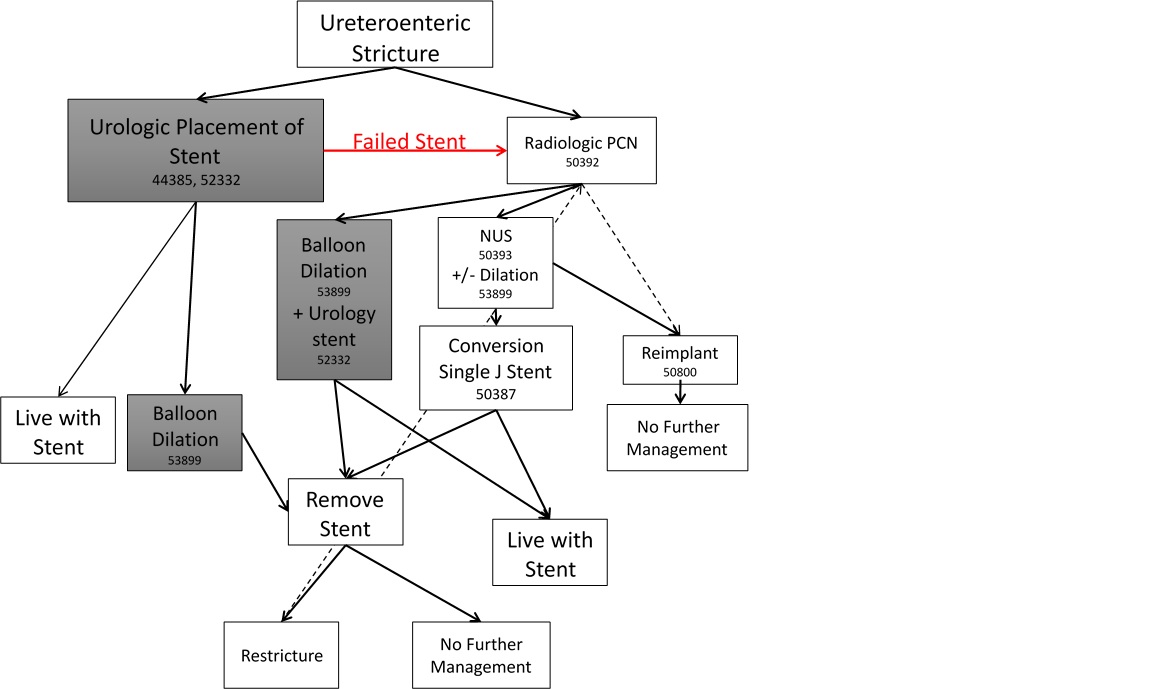
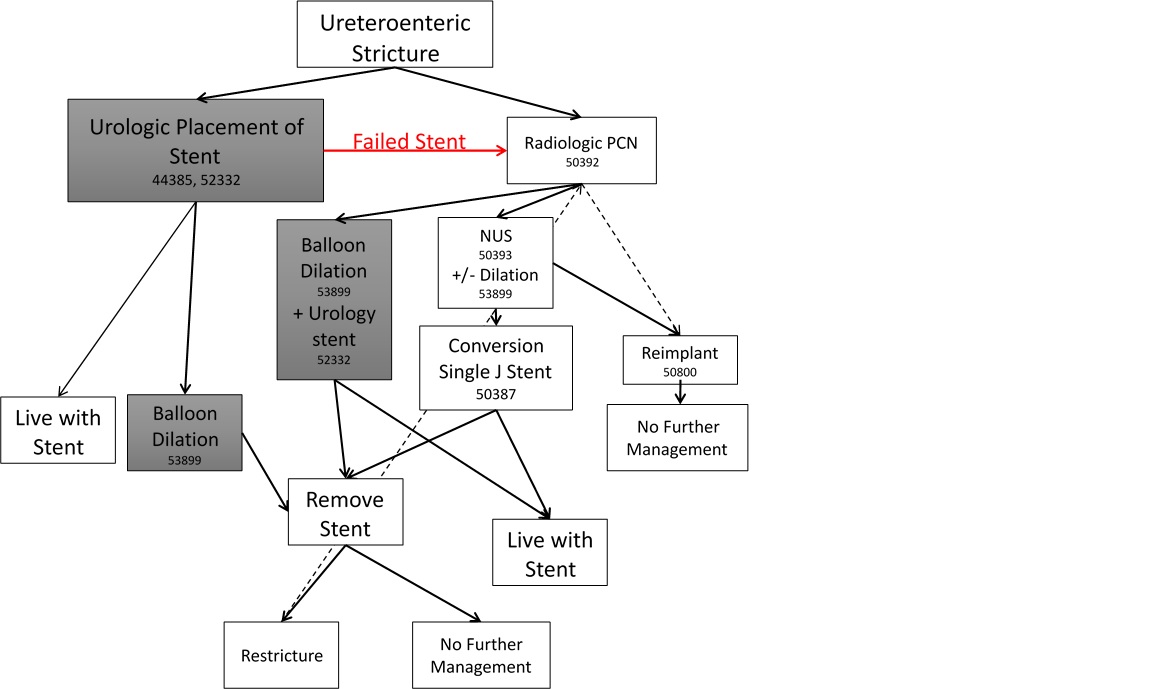
Methods:Primary outcome measures were stricture management time and cost based on 2014 Medicare CPT reimbursement rates. We built a simulation model (Figure 1) using Arena Simulation Software simulating the experience of 1000 patients. The model describes three outcomes: urologic stent placement, PCN, and failed urologic management requiring PCN. The percentage of patients pursuing each treatment arm, average time to from stricture to clinical stability, and failure rate are modeled on a review of relevant literature and clinic experience
Results: Urologic retrograde stent placement efficacy was modeled at 50%. Patients who pursued initial urologic management incurred an average cost of \.13 and management time of 142 days. This includes patients who only required urologic treatment (\.39, 141 days) and those who failed and required PCN (\.16, 143 days). Initial PCN alone cost \.00 and had the longest management time (152 days). Sensitivity analysis showed that a urologic success rate as low as 15% still favored initial urologic approach based on lower cost and management time.
Conclusion: Our model predicts a time and cost advantage to initial urologic management. Urologists should consider this strategy.
Back to 2015 Joint Annual Meeting
|