|
Back to 2014 Annual Meeting Abstracts
Fast Track Pathway for Nephrectomies: Expediting Hospital Discharges for Renal Surgery
Maria Voznesensky, M.D.1, Christopher Mutter, B.A.2, Lisa Beaule, MD1, Matthew Hayn, MD1.
1Maine Medical Center, South Portland, ME, USA, 2Rocky Vista University, Parker, CO, USA.
BACKGROUND: In this study, we outline our current postoperative treatment of patients undergoing renal surgery (robotic, laparoscopic) which allows for early institution of an oral diet and early hospital discharge. We describe overall improvement in patient recovery and outcomes after institution of the ‘fast track’ discharge program.
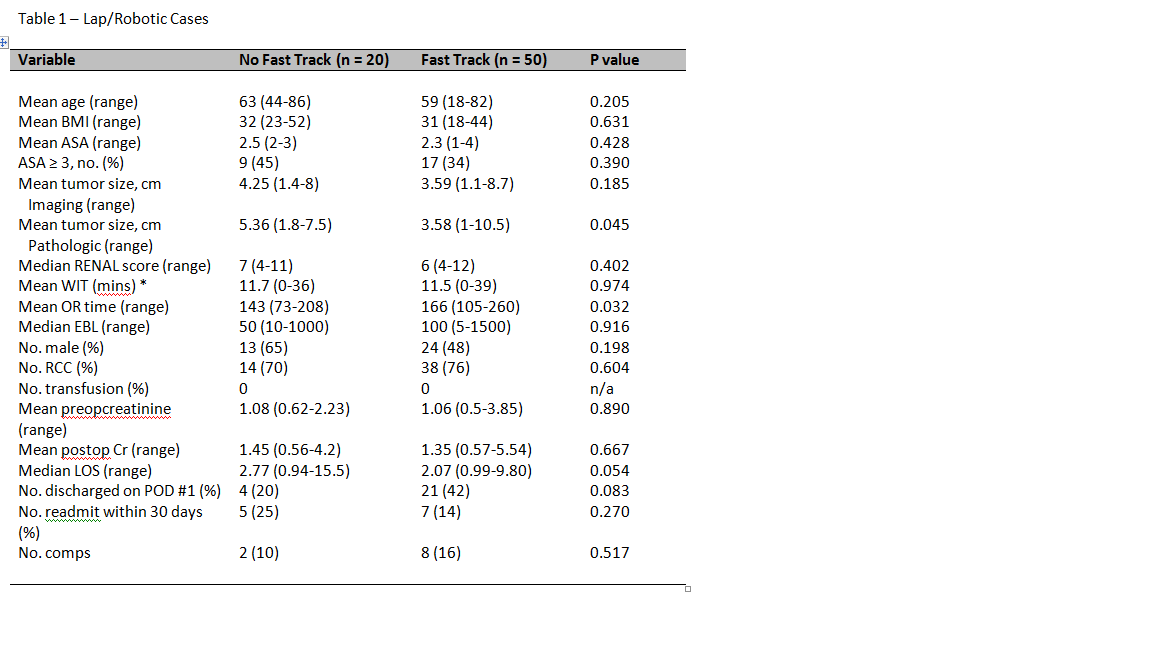
METHODS: 50 consecutive patients underwent renal surgery from June 2013 to Jan 2014. This included laparoscopic nephrectomy, robotic laparoscopic partial nephrectomy, and robotic laparoscopic radical nephrectomy. The results of the current series were compared to a 20 patient control group managed consecutively, 6 months prior to the institution of the fast track clinical pathway. A care plan was followed for all fast track patients and included the use of non-narcotic analgesics, early institution of an oral diet, ambulation on post op day zero, and early catheter removal. The outcomes with regard to time to hospital discharge were assessed.
RESULTS: A total of 50 consecutive renal surgery patients received fast track clinical pathway care. Mean patient age was 59 years (range, 18-82 years), and body mass index was 31 kg/m(2) (range, 18-44 kg/m(2)). Mean tumor size was 3.59 cm (range, 1.1-8.7 cm), and mean RENAL nephrometry score was 6 (range, 4-12). Mean warm ischemia time was 11.5 minutes (range, 0-39 minutes). The mean surgical time was 2.7 hours, and the mean estimated blood loss was 100 mL. Mean preoperative and discharge creatinine were 1.06 mg/dL (range0.5-3.85 mg/dL) and 1.35 mg/dL (range, 0.57-5.54 mg/dL) respectively. Mean length of stay was 2.07 days, with 21 (42%) discharged on post-operative day one. Median length of stay was shorter in the fast track group than in the controls (2.07 days vs. 2.77 days, p= 0.054). 7 (14 %) were readmitted within 30 days. 8 (16%) patients had delayed complications.
CONCLUSIONS: Advancements in postoperative management have been successfully used in our patient population to allow for early hospital discharge in laparoscopic and robotic nephrectomy cases. Readmission and complication rates were low indicating that this protocol is safe and effective.
Back to 2014 Annual Meeting Abstracts
|

|

