|
Back to 2014 Annual Meeting Abstracts
Intravesical Hemostatic Clip Migration After Robotic Prostatectomy; Case Series and Review of the Literature
Joseph M. Brito, III, MD, Andrew Leone, MD, George A. Turini, III, MD, Dragan J. Golijanin, MD, E. Bradley Miller, MD, Gyan Pareek, MD, Joseph F. Renzulli, MD.
Warren Alpert Medical School at Brown University, Providence, RI, USA.
BACKGROUND: The Weck Hem-o-lock Ligating Clip is a routinely used hemostatic tool in robotic surgery. It has been the practice in our institution to use such clips for hemostasis of the vascular pedicles during robotic prostatectomy. Migration of such clips has been reported in the literature as case reports. Here we present a series of intravesical weck clip migration.
METHODS: A retrospective chart review was conducted over the period 2006-2011. Patients were drawn from a robotic prostatectomy database at a single institution. The study group required cystoscopic intervention for removal of clips. Primary datapoint was type of intervention required (laser lithotripsy, lithalopaxy, or simple extraction). Length of initial postoperative hospital stay, operative time, Gleason grade, patient age, blood loss and tumor stage were also investigated.
RESULTS: Of 570 total prostatectomies, (1.4%) required return to OR. Extraction methods included laser lithotripsy, blunt lithalopaxy and grasper extraction. One patient required more than one intervention for clip removal. Differences in average Gleason grade, console time, estimated blood loss, and patient age were not significant. Increased length of hospital stay and need for PRBC transfusion were significantly associated with clip migration. The most common pathologic stage was pT2 and did not differ between groups. Average time to presentation after initial surgery was 1.75 years.
CONCLUSIONS: Weck clip migration is a recognized potential complication of robotic assisted radical prostatectomy. Banks et al initially identified this complication following laparoscopic prostatectomy in 2008. Clip migration should be considered for post-RALRP patients with recurrent UTI, dysuria, or hematuria. One clip located at the bladder neck was removed in the office, however in general migrated clips required return to the OR where anesthesia and fulguration of bleeding sites could be performed. Operative time and gleason grade did not appear to be a factor in clip migration. Interestingly, patients who subsequently had clip migration into the bladder had a longer average hospital stay after RALRP. One reason for longer stay in the migration group was increased incidence of red cell transfusion. We postulate that clip migration may be an early event in this subpopulation causing increased postoperative blood loss and possibly allowing early incorporation of the clip into the bladder neck anastomosis. We recommend judicious use of hem-o-lock clips and have begun employing these clips only for neurovascular pedicle hemostasis. Given the delay in presentation from initial surgery to presentation, longitudinal research is needed to determine if this change in surgical technique is effective in mitigating clip migration.
Characteristics of Control and Clip Migration Groups | Control Group | Clip Migration Group | p-Value | | Gleason Grade | 6.6 | 6.8 | 0.29 | | Console Time (min | 170.6 | 173.5 | 0.44 | | Estimated Blood Loss (mL) | 260 | 240 | 0.31 | | Patient Age (years) | 60.2 | 62.4 | 0.22 | | Length of Stay (days) | 2.02 | 7.6 | <0.01 | | PRBC Transfusion (units) | 0.05 | 1.4 | <0.01 | 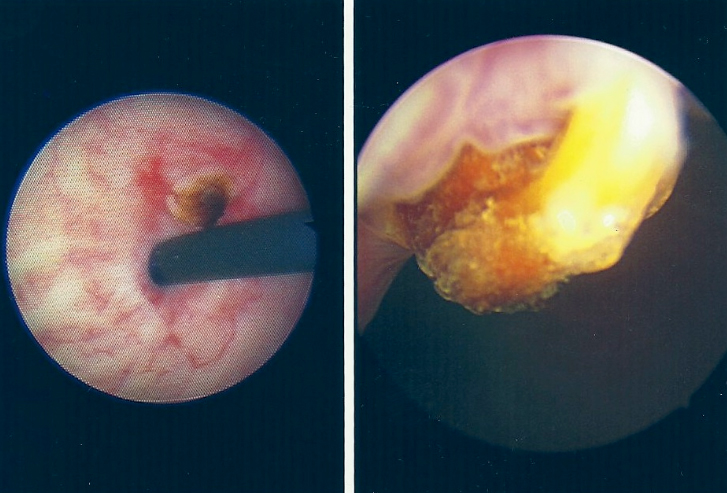 
Back to 2014 Annual Meeting Abstracts
|

|

