|
Back to 2014 Annual Meeting Abstracts
Robotic assisted Laparoscopic Partial Nephrectomy (RALPN) for Clinical T1b Renal Masses: A Retrospective Cohort Review
Andrew Leone, MD, George Turini, MD, Timothy Tran, MD, Joseph Renzulli, MD, Gyan Pareek, MD, Dragan Golijanin, MD.
Warren Alpert Medical School at Brown University, Providence, RI, USA.
INTRODUCTION: Robotic assisted laparoscopic partial nephrectomy (RALPN) has become the standard of care in the management of small renal masses. Nephron sparing surgery has expanded to include management of larger renal masses including clinical T1b renal masses. We aimed to evaluate the safety, efficacy, and oncologic outcome of RALPN for clinical T1b renal masses.
METHODS: 119 patients who underwent robotic partial nephrectomy by a single surgeon at our institution from 2011 to 2014 were retrospectively reviewed. This cohort included 21 patients with clinical T1b renal masses (>4 cm). Perioperative parameters including clinical renal mass size and demographic data were obtained from chart review. Using Student's t-test and Fisher's exact test perioperative and demographic data were compared between clinical T1b and T1a patients who underwent RALPN.
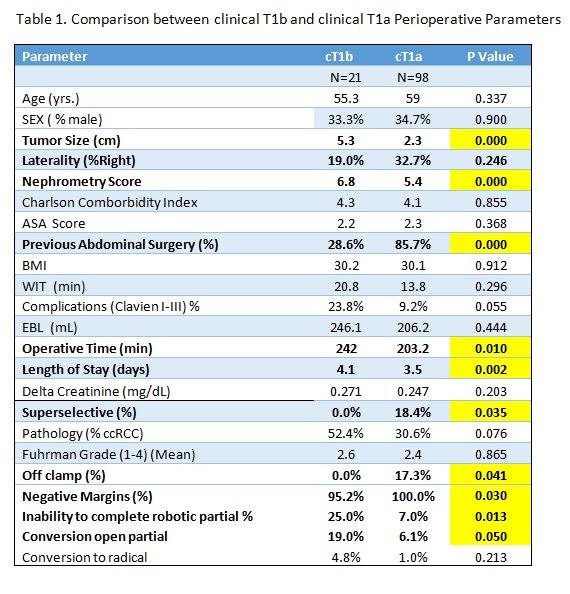
RESULTS: Clinical T1b vs. clinical T1a patients' demographic and perioperative data were compared (Table 1). For clinical T1b patients tumor size (5.3 cm vs. 2.3 cm, p<0.0001) R.E.N.A.L nephrometry score (6.8 vs. 5.4, p = 0.009), and previous abdominal surgery (29 % vs. 86 % p<0.0001) were all significantly different. Perioperative parameters that were statistically significant were operative time (242 min vs. 203 min, p=0.010) and length of hospital stay (4.1 days vs 3.5 days, p= 0.002). There were no off-clamp or superselective clamping performed in clinical T1b patients compared to 18% of clinical T1a and 17% T1b respectively. Only one in the clinical T1b cohort had positive margins compared to zero in the T1a cohort (p = 0.03). Delta creatinine at 3 months postoperatively was not statistically significant between the patients. Inability to complete robotic partial was more common in the T1b cohort 25% vs. 7% in the T1a cohort (p=0.030) including a statistically significant difference in conversion to open partial (because of location of tumor, or size of tumor) 19% vs. 6.1% (p=0.050). Clavien I-III complications were not statistically significantly different although a greater percentage of patients in the T1b cohort had complications (24% vs. 9% p=0.055). Pathology was not statistically different although more patients in the T1b cohort had clear cell RCC 52% vs. 32% (p=0.076). Fuhrman nuclear grade was equivalent with the median grade 2.6 vs. 2.4 (p=0.865).
CONCLUSIONS: RALPN for patients with clinical T1b renal masses is safe and efficacious for select patients. However, operative time and hospital stay were longer for patients with clinical T1b masses as well as need to convert to open partial nephrectomy. When counseling patients with clinical T1b renal masses, RALPN should be considered as a feasible option in select patients.
Back to 2014 Annual Meeting Abstracts
|

|

