|
Back to 2014 Annual Meeting Abstracts
Patient-Reported Quality of Life and Convalescence Outcomes after Minimally Invasive Partial and Radical Nephrectomy
Peter Chang, MD, Tudor Borza, MD, Jialin Mao, MPH, Arie Carneiro, MD, Andrew Percy, BS, Catrina Crociani, MPH, Kimberly Taylor, BA, Srikanth Vedachalam, BA, Andrew Wagner, MD.
Beth Israel Deaconess Medical Center, Boston, MA, USA.
BACKGROUND:
AUA guidelines now recommend PN whenever surgically feasible for treatment of renal masses. While oncologically effective, PN has been
associated with a higher peri-operative complication rate and longer hospital stay than RN, likely because of its higher relative procedural complexity. It has yet to be determined whether there are differences in patient-reported quality-of-life and convalescence outcomes between RN and PN. We aim to investigate this question using a prospective longitudinal study.
METHODS: We enrolled subjects who underwent laparoscopic/robot-assisted partial nephrectomy or laparoscopic radical nephrectomy and provided informed consent to an IRB-approved prospective quality-of-life study at our institution. Subjects received SF-12 and Convalescence and Recovery Evaluation (CARE) questionnaires at pre-treatment baseline
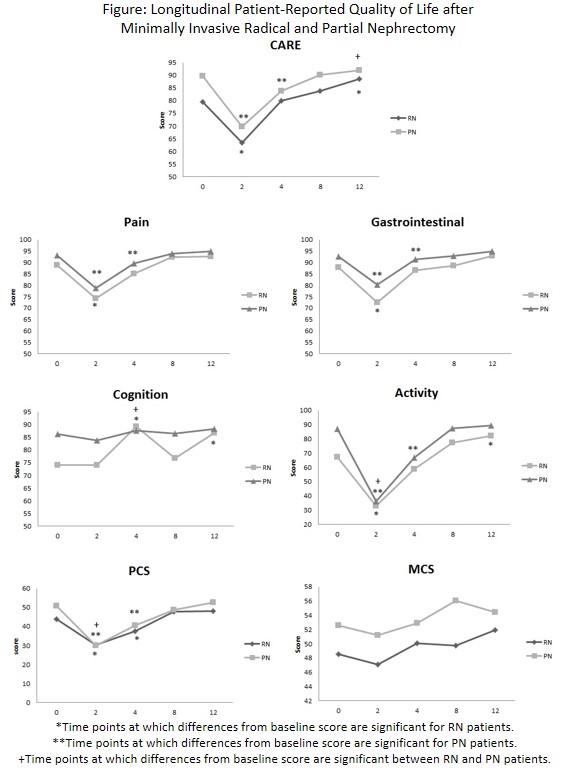
and 2, 4, 8, and 12 weeks post-treatment. SF-12 is comprised of mental and physical component subscales, while CARE contains Pain, Gastrointestinal, Cognition, and Activity subscales, as well as an overall CARE score. After excluding subjects with evidence of metastatic disease and those without baseline information, we compared baseline patient demographics and clinical characteristics between groups. We then performed longitudinal analysis using a mixed repeated measures model to assess time effect within each surgery group and to evaluate the association between type of surgery received and post-surgery quality of life.
RESULTS: Eighty (69%) PN and 36 (31%) RN subjects were included in the analysis. Mean tumor size was 2.7 cm for PN, and 8.1 cm for RN subjects. There were no significant differences in age, BMI, or Charlson score between groups, but PN subjects had significantly higher overall CARE score, gastrointestinal, cognition, activity and SF-12 physical composite score (PCS) and mental composite score (MCS) than RN subjects at pre-treatment baseline. At 2 weeks, both groups showed significant decreases in overall CARE score, Pain, Gastrointestinal, Activity and SF-12 PCS, with PN subjects experiencing worse relative decline in Activity and SF-12 PCS, reaching scores equivalent to RN subjects (Figure). Differences in overall CARE, Pain, Gastrointestinal, and Activity at 4 weeks remained significant for PN, while RN subjects had returned to baseline. By 8 weeks post-treatment, all metrics had returned to baseline for both groups. RN subjects showed continued improvement such that 12 week scores were higher than baseline in all categories, though this was significant only for overall CARE, Cognition and Activity scores.
CONCLUSIONS: Subjects selected to undergo partial nephrectomy have better baseline patient-reported HRQOL than radical nephrectomy subjects, and experience greater relative declines in patient-reported Activity and SF-12 physical scores in the immediate post-surgical period, with scores reaching levels equivalent to RN subjects. 4-8 week convalescence is similar between the two groups, with both groups returning to baseline by 8 weeks, and statistically significant changes between groups likely driven by differences in baseline scores. Radical nephrectomy subjects experience overall longer-term improvement of quality of life beyond baseline scores.
Back to 2014 Annual Meeting Abstracts
|

|

