|
Back to 2014 Annual Meeting Abstracts
Circumcision Status and HIV, HSV and HPV: A Contemporary Analysis of U.S. Men Using the National Health and Nutrition Survey (NHANES).
Briony K. Varda, Medicine1, Philip J. Cheng, MD1, Marc Cendron, MD2, Steven L. Chang, MD, MS1.
1Brigham and Women's Hospital, Boston, MA, USA, 2Boston Children's Hospital, Boston, MA, USA.
Introduction
Randomized controlled trials based in Africa report that male circumcision confers a protective effect against acquiring human immunodeficiency virus (HIV), herpes simplex virus (HSV), and human papillomavirus (HPV). The applicability of these findings in the United States (US) is unclear. This contemporary population-based study evaluates the relationship between circumcision and HIV, HSV, and HPV seropositivity in the US.
Methods
Data from men 14- to 59-years of age was pooled for 2003 to 2010 of the National Health and Nutrition Examination Survey (NHANES). We developed multivariable logistic regression models to evaluate the relationship between circumcision status and HIV, HSV, and HPV controlling for relevant clinical and sociodemographic factors that potentially alter the risk of viral acquisition. We used multiple imputation to account for survey nonresponse, employed propensity weighting to correct for a selection bias for circumcision, and adjusted for survey weighting to achieve a nationally representative sample.
Results
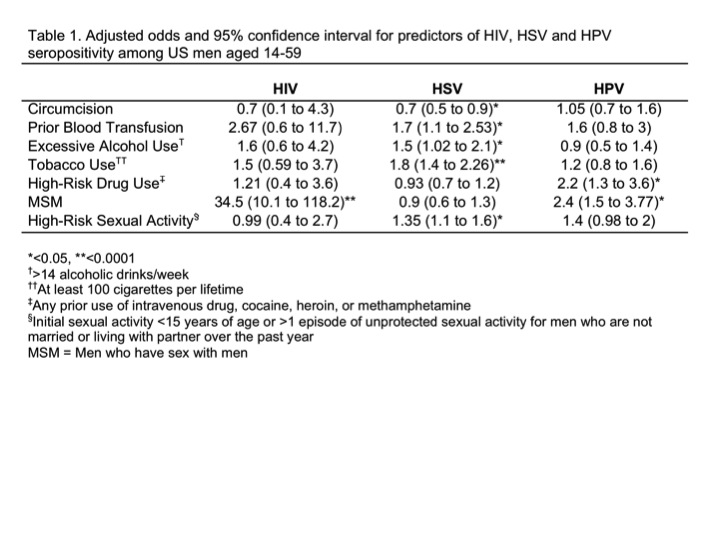
A total of 9,388 men were included with a weighted sample size of 90,967,232. The majority of men reported being circumcised (80.3%). This was most common for men who were Caucasian (90.6%), born in the US (87.6%), in the highest income category (≥$75,000, 88.3%), with greater than a high school education (85.8%), and with health insurance (83%). Seropositivity for HIV, HSV, and HPV was 0.7%, 61.8%, and 14.3%, respectively. After controlling for prior blood transfusions and risk behaviors (alcohol, tobacco, illicit drug, and sexual activity), we found that that circumcision was associated with lower odds of HSV (OR 0.7, p<0.05) but was not a predictor of HIV and HPV seropositivity among the men in our cohort (Table 1).
Conclusions
In the US, circumcision has no association with HIV and HPV seropositivity rates among males, which potentially relates to the relatively low prevalence of HIV and high clearance of HPV. Circumcision is associated with a lower likelihood of HSV2 infection. Clinical trials focused on understanding the effect of circumcision on the risk reduction of STI acquisition in the US are needed.
Back to 2014 Annual Meeting Abstracts
|

|

