|
Back to 2014 Annual Meeting Abstracts
Fournier’s Gangrene (FG): A Multidisciplinary Approach since 2011 at an Academic Level 1 Trauma Center Improves Patient Survival
Andrew R. Leone, MD1, George A. Turini, MD1, Andrew Tompkins, MD1, Atip Chatsudthipong, MD1, David Harrington, MD2, Kennon Miller, MD1, Pamela Ellsworth, MD3.
1Brown/RIH Urology, Providence, RI, USA, 2Brown University General Surgery, Providence, RI, USA, 3UMass Medical Center, Worcester, MA, USA.
BACKGROUND
In 2011, the Urology, Trauma and Critical Care Services developed and instituted a multidisciplinary approach to the management of Fournier's Gangrene as a Quality Improvement initiative. We sought to evaluate our experience with this initiative and determine its impact on patient care and outcomes.
METHODS
An IRB approved retrospective review of all patients (n=29) treated at Rhode Island Hospital between 2011-2014 with
Fournier's Gangrene (FG) was performed. The multidisciplinary approach involved simultaneous consultation of the Urologic and Trauma Surgery services in the emergency room and the presence of both services at the time of surgical debridement. Postoperative care was assigned to the Critical Care Service, with the Urology team following in consultation. Demographic parameters and perioperative measures were reviewed via electronic medical record. Patients treated at Rhode Island Hospital with Fournier’s Gangrene from 2008-2010 were used as a comparison group to compare outcomes from prior to implementation of the multidisciplinary protocol.
RESULTS -
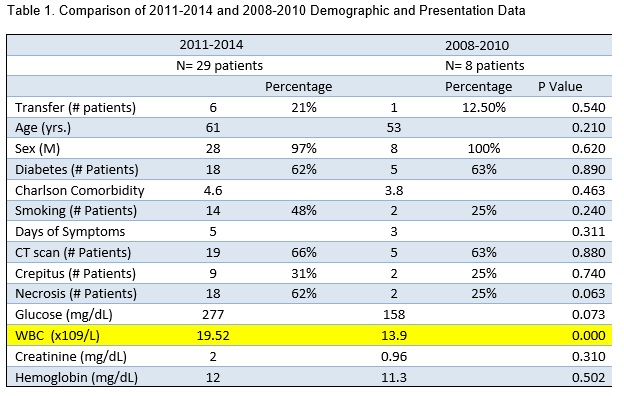
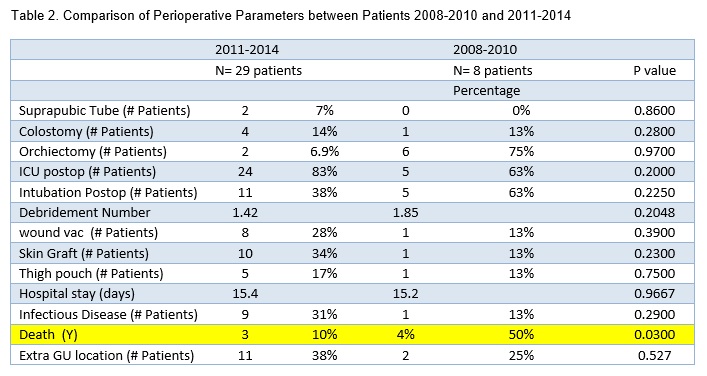
Of 29 patients from 2011-2014, 93% (27/29 patients) underwent operative management of FG since implementation of the multidisciplinary approach at our institution. From 2008 to 2010, eight patients underwent debridement for Fournier’s Gangrene. From 2011-2014 six patients (21%) were transferred from outside hospitals while in 2008-2010 only 1 patient (12.5%) was transferred (p=0.540). Demographic and presentation data (Table 1) were compared between the two cohorts including age, gender, presence of diabetes, Charlson comorbidity index, smoking, days of symptoms, physical exam findings (crepitus, necrosis), presence of CT imaging and laboratory data (Glucose, WBC, Creatinine, Hemoglobin). Only WBC was statistically significantly different between the two cohorts (19.5 vs 13.9, p= < 0.0001). Perioperative and outcomes data were compared between the two cohorts (Table 2). There was a statistically significant decrease in all-cause mortality in the multdisciplinary cohort (2011-2014) evidenced by only 3 deaths in those patients compared to 4 in the earlier cohort of patients (2008-2010) (p=0.03). Other parameters including number of surgical debridements, need for suprapubic tube, colostomy, orchiectomy, skin grafting, intubation, wound vac, skin graft, thigh pouch, length of hospital stay, infectious disease consultation, and extra genitourinary involvement were not statistically different.
CONCLUSIONS - We reviewed our experience with a multidisciplinary approach to patients presenting with FG which optimizes patients’ access to excellent surgical and postoperative care which is critical in ensuring optimal outcomes in this morbid urologic emergency. Multidisciplinary management significantly improved all-cause mortality. Compared to a cohort of patients in the three years prior to implementation we observed similar presentation and demographic data with a significantly lower mortality in the cohort of patients undergoing multidisciplinary management.
Back to 2014 Annual Meeting Abstracts
|

|

