|
Back to 2014 Annual Meeting Abstracts
Trends in the Surgical Approach for Adolescent Varicocelectomy
Miriam Harel, MD1, Katherine W. Herbst, MSc2, Eric Nelson, MD1.
1Connecticut Children's Medical Center/University of Connecticut Health Center, Hartford/Farmington, CT, USA, 2Connecticut Children's Medical Center, Hartford, CT, USA.
Background:
The indications for surgical intervention in adolescent patients with varicocele as well as the ideal surgical approach remain controversial. While the subinguinal microsurgical approach appears to have become the gold standard for varicocele ligation in adult males with infertility, this approach has not been widely adopted in the adolescent population.
In this study, we sought to describe recent trends in the choice of surgical approach for adolescent varicocelectomy using the Pediatric Health Information System (PHIS) database.
Methods:
Hospitals enrolled in the PHIS database that reported outpatient surgeries by Current Procedural Terminology (CPT) code from 2003 to 2012 were included. Since not all procedures are reported by CPT code, the number of procedures reported by the International Classification of Diseases-9 (ICD-9) codes were compared to the number of procedures reported by CPT code for each year. In order to provide quality control of the dataset, hospitals that did not report all procedures by CPT code were excluded for that particular year.
Patients at least ten years of age whose records contained both the ICD-9 code for varicocele (456.4) and a CPT code for varicocelectomy [55550 (laparoscopic), 55530 (open inguinal), 55535 (open abdominal)] were identified. Microsurgical approach was identified by CPT code 69990. Patients undergoing concurrent hernia or hydrocele repair were excluded.
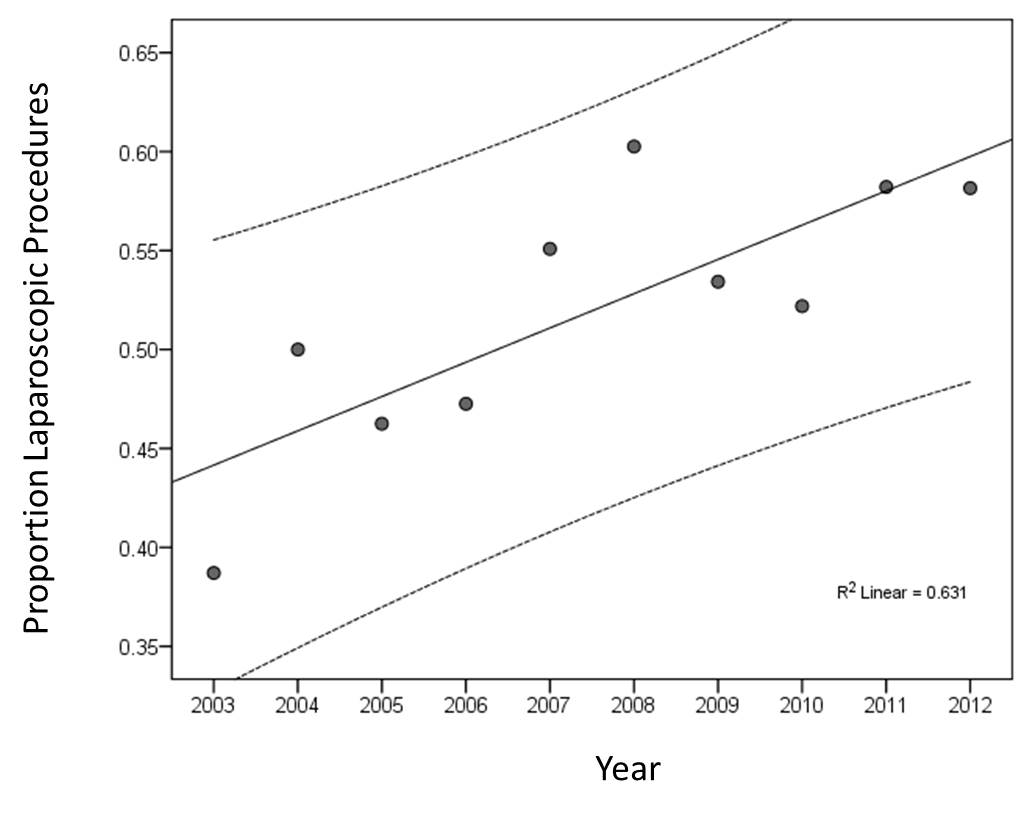
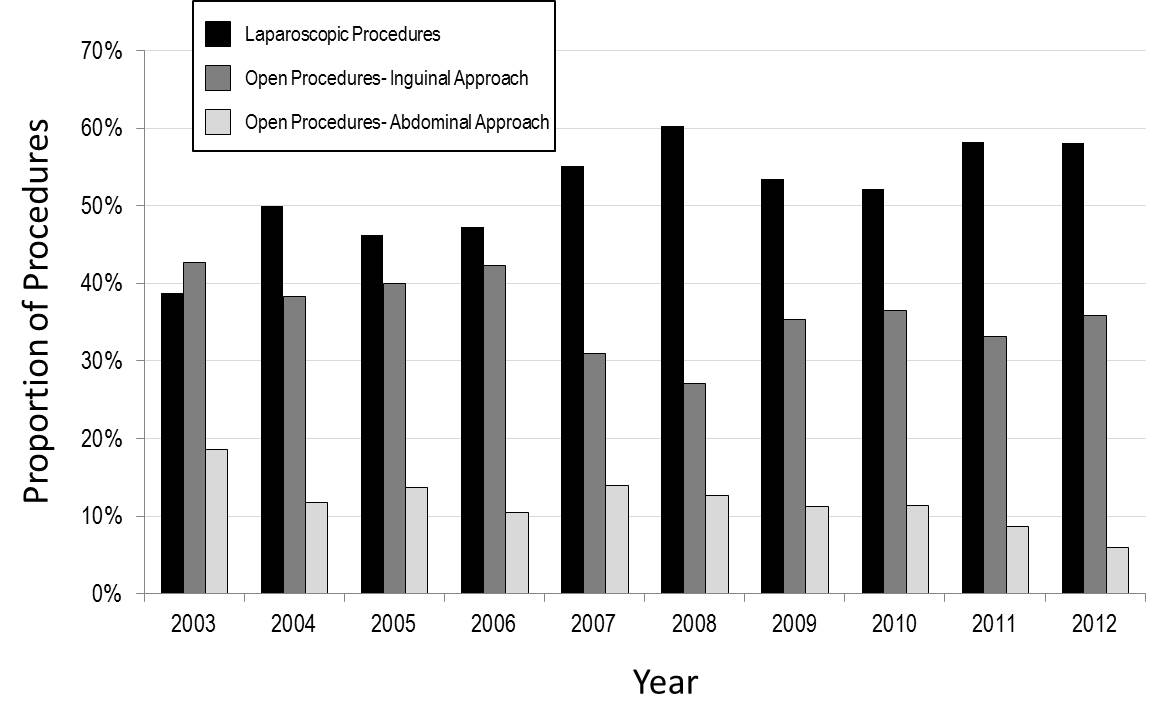
Linear regression analysis was used to describe trends across time.
Results:
The number of hospitals that met the inclusion criteria increased from 15 hospitals in 2003 to 33 in 2012. After excluding 117 patients who underwent concurrent hernia or hydrocele repair and 78 records from hospitals underreporting ambulatory surgeries by CPT code, a final cohort of 2,528 patients was identified. Mean age was 15 years. (+ 2 years)
Over half (53.6%) of reported varicocelectomies were performed laparoscopically. Of the remaining open surgeries, 76.3% were performed with an inguinal/subinguinal approach, and 23.7% were approached abdominally. A microsurgical approach was reported in only 2% of open varicocelectomies. (21 inguinal/subinguinal, 2 abdominal)
Linear regression demonstrated that the proportion of laparoscopic varicocelectomies significantly increased over the study period. (R2=0.63, p<0.01) (Figure 1) With each additional year, the proportion of laparoscopic procedures increased by approximately 1.7%. The proportion of abdominal varicocelectomies significantly declined over the study period (R2=0.64, p<0.01), decreasing by approximately 0.9% with each additional year. The proportion of inguinal surgeries did not change significantly. (R2=0.27, p=0.12) (Figure 2)
Conclusions:
We identified a trend of increasing use of a laparoscopic approach for adolescent varicocelectomy, which appears to be driven mostly by a transition from open abdominal surgery. While subinguinal microsurgical repair appears to have become the gold standard for management of varicoceles in adult males with infertility, this technique was infrequently reported within this adolescent cohort.
Back to 2014 Annual Meeting Abstracts
|

|

