|
Back to 2014 Annual Meeting Abstracts
Variation Among Hospitals and Surgeons in Bilateral Endoscopic Treatment of Primary Vesicoureteral Reflux (VUR)
John H. Makari, MD, MHA, MA1, Katherine W. Herbst, MSc2, Sean T. Corbett, MD3, James I. Hagadorn, MD1, Anthony A. Caldamone, MD4, Thomas S. Lendvay, MD5.
1Connecticut Children's Medical Center/UConn School of Medicine, Hartford/Farmington, CT, USA, 2Connecticut Children's Medical Center, Hartford, CT, USA, 3University of Virginia Children's Hospital/University of Virginia School of Medicine, Charlottesville, VA, USA, 4Hasbro Children’s Hospital/Brown University School of Medicine, Providence, RI, USA, 5Seattle Children’s Hospital/University of Washington School of Medicine, Seattle, WA, USA.
Background:
Indications for bilateral, rather than unilateral, surgical intervention for VUR include the radiographic presence of bilateral VUR or risk factors thought to increase the risk of development of contralateral VUR after treatment of unilateral VUR, such as a history of bilateral VUR or an abnormal configuration or position of the contralateral ureteral orifice. The purpose of this study was to examine variation among US surgeons’ and freestanding children’s hospitals’ utilization of bilateral endoscopic treatment of primary VUR using administrative data to better understand current surgical practice.
Methods:
The Pediatric Health Information System (PHIS) database was queried (2009 to 2012) for outpatient records reporting both a diagnosis of VUR and initial endoscopic injection for treatment of VUR. Hospitals reporting <80% of ambulatory surgery cases by CPT code, not coding for bilateral injection, or with 18 years were excluded. Bilateral intervention was defined as either CPT Code modifier 50 or two entries of CPT code 52327 on the same admission. Surgeons with <5 procedures during the study period were excluded from surgeon-level variation analysis. Univariate and multivariate analyses of non-independent data were performed with hierarchical linear or logistic regression.
Results:
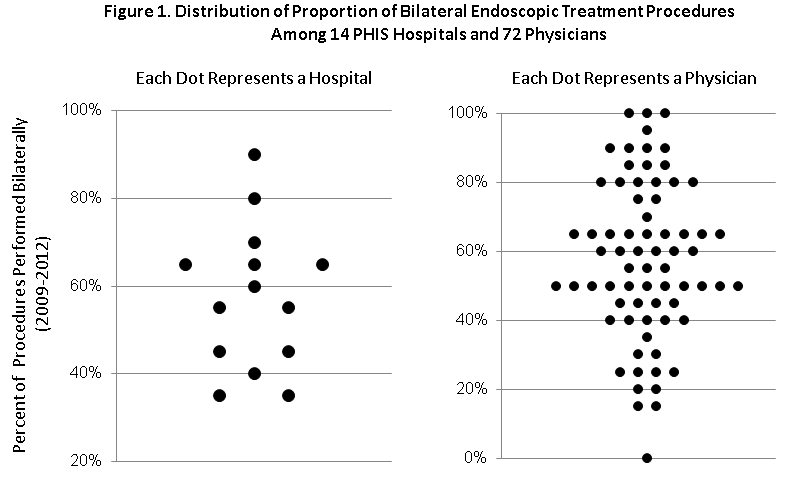
After applying exclusion criteria, records of 2,111 patients undergoing endoscopic treatment of VUR by 96 surgeons at 14 hospitals were identified. Over half the cohort (59%) underwent bilateral interventions. Proportion of bilateral procedures varied almost three fold among hospitals, and 10 fold among surgeons. (Fig. 1) Variation among hospitals accounted for 70% of total variation, and among surgeons within hospitals, 30% of total variation. Multivariate analysis, adjusting for univariate significant factors, found age at intervention [OR 0.93 (p<0.001)] and public insurance [OR 0.58 (p<0.001)] significantly associated with bilateral treatment, with odds of undergoing bilateral treatment reduced 7% with each additional year of age and 42% if publically insured.
Conclusions:
In this cohort, there was wide variation among hospitals and among surgeons within hospitals in the proportion of patients undergoing bilateral endoscopic treatment of VUR. Absence of laterality-specific diagnosis codes and of published bilateral VUR prevalence precluded identifying the degree to which these results reflect treatment of actual bilateral disease versus risk of contralateral development; bilateral disease prevalence should not vary by geography alone, so it should not explain variation in surgeon and institutional utilization. Further investigation into variation in open, laparoscopic and robotic-assisted bilateral surgical intervention for VUR may serve to provide better understanding of the influence of treatment modality on bilateral surgical intervention.
Back to 2014 Annual Meeting Abstracts
|

|

