|
Back to 2014 Annual Meeting Abstracts
“How are you REALLY doing?”: Assessing and Reporting Longitudinal Patient-reported Prostate Cancer Outcomes Collected at the Point of Care using EPIC for Clinical Practice (EPIC-CP)
Peter Chang, MD, MPH1, Arie Carneiro, MD1, Kimberly Taylor, BA1, Srikanth Vedachalam, BA1, Catrina Crociani, MPH1, Martin G. Sanda, MD2, Andrew A. Wagner, MD1.
1Beth Israel Deaconess Medical Center, Boston, MA, USA, 2Emory University, Atlanta, GA, USA.
Background: Practitioners tend to underestimate the severity of patients’ treatment-related side effects and overestimate their own rates of favorable patient outcomes. Therefore, the question “how are you REALLY doing?” is applicable to both patient and practitioner in prostate cancer care, and can be objectively answered only through consistent, longitudinal assessment of patient-reported outcomes. We developed the Expanded Prostate Cancer Index Composite for Clinical Practice (EPIC-CP) specifically to facilitate prostate cancer-related HRQOL assessment at the point-of-care (Chang P et al, J Urol Sep 2011). Herein we present the first ever report of longitudinal prostate cancer outcomes collected in routine urologic practice using EPIC-CP.
Methods: We reviewed practitioner-reported and patient-reported HRQOL outcomes using EPIC-CP in 202 patients who underwent robot-assisted radical prostatectomy from June 2010 to June 2013 with three surgeons at our institution. EPIC-CP is scored similarly to the AUA Symptom Index (domain item answers summed, higher score = worse HRQOL) and also includes common clinical questions (e.g., incontinence pads, functional erections, etc). We used the paired t-test and Wilcoxon signed-rank test to compare domain scores between baseline and 3, 6, and 12 months post-treatment. We considered p-values < 0.05 statistically significant and domain score changes greater than the published minimally important differences (Chipman et al J Urol Mar 2013) clinically significant.
Results: We began administering EPIC-CP in July 2010, and by September 2011, every prostate cancer patient completed EPIC-CP pre- and post-treatment in the waiting room on paper. All questionnaires were scored immediately and used to facilitate clinical counseling within routine practice flow without research personnel.
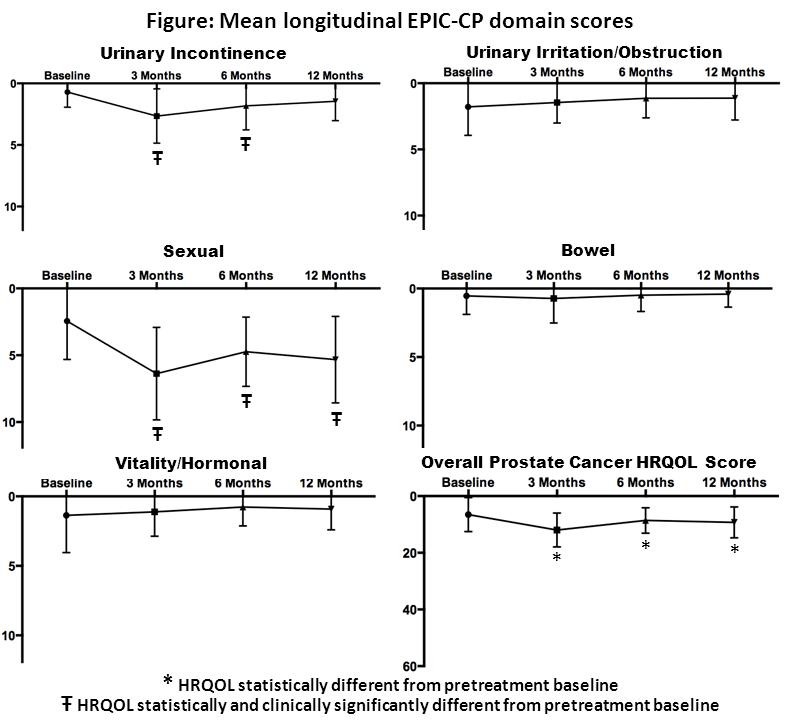
389 EPIC-CP questionnaires were completed. Mean urinary incontinence scores increased (worsened) significantly 3 and 6 months post-treatment, but returned to baseline at 12 months (Figure). Using EPIC-CP, 47%, 76%, and 78% of patients reported no incontinence pad use at 3, 6, and 12 months post-treatment, respectively, which was consistent with our practitioner-reported rates and previous patient-reported rates in a multicenter prospective study (76% in Sanda et al NEJM 2008). Mean sexual scores worsened after surgery, and differences remained statistically and clinically significant at 12 months (Figure). While practitioners reported that 56% of patients had erections sufficient for intercourse at 12 months, patient-reported functional erection rates with EPIC-CP were lower (28%), and consistent with existing patient-reported rates (25% in Sanda et al). Bowel and vitality/hormonal domain scores were unchanged over time, and urinary irritation/obstruction scores trended towards improvement after surgery (Figure).
Conclusions: This study is the first to demonstrate the feasibility of longitudinal prostate cancer patient-reported outcome assessment in the routine practice setting using EPIC-CP. Our results using EPIC-CP are consistent with previous well-established patient-reported outcomes collected using EPIC-26. We believe this study exemplifies how routine PRO use in clinical care is necessary for us to objectively ask how our patients are doing with their treatment recovery (or lack thereof), and how we are really doing as providers.
Back to 2014 Annual Meeting Abstracts
|

|

