|
Back to 2014 Annual Meeting Abstracts
POSTOPERATIVE COMPLICATIONS OF RADICAL NEPHRECTOMY WITH ATRIAL THROMBECTOMY: A CONTEMPORARY POPULATION-BASED ANALYSIS
Tudor Borza, MD1, Jeffrey Leow, MBBS, MPH1, Benjamin Chung, MD2, Steven Chang, MD, MS1.
1Brigham and Women's, Boston, MA, USA, 2Stanford University Medical Center, Palo Alto, CA, USA.
BACKGROUND:
The mainstay treatment for patients with stage T3c renal cell carcinoma (RCC) is a radical nephrectomy with atrial thrombectomy (RN−AT).
Although this procedure is widely recognized to have substantial morbidity and mortality, little data exist on the actual rates of postoperative complications. Using a contemporary population−based cohort, we sought to determine the postoperative complication rate among patients undergoing RN−AT.
METHODS:
We queried the Premier Hospital Database (Premier, Inc, Charlotte,
NC) to identify patients that underwent nephrectomy (ICD9 55.51) between January 1, 2003 and December 31, 2012. We limited our analysis to patients who concurrently underwent cardiopulmonary
bypass, determined through billing codes, as these patients were assumed to have undergone a RN−AT. We captured patient and hospital data as well as determined 90−day postoperative complications defined by the ClavienClassification System through review of ICD9 codes and disposition data.
RESULTS:
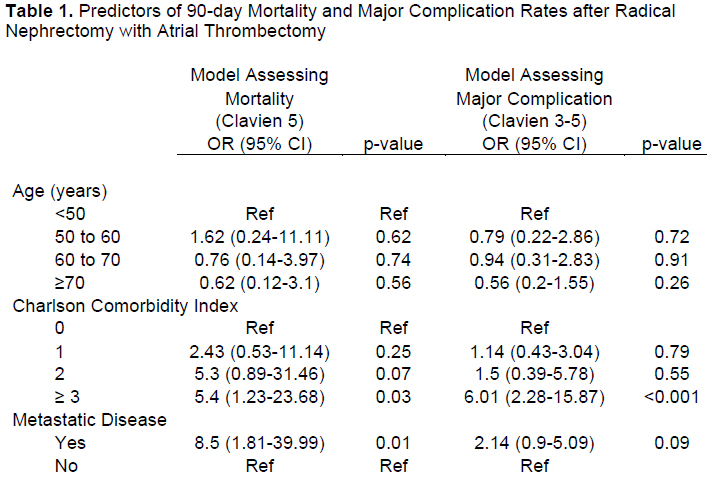
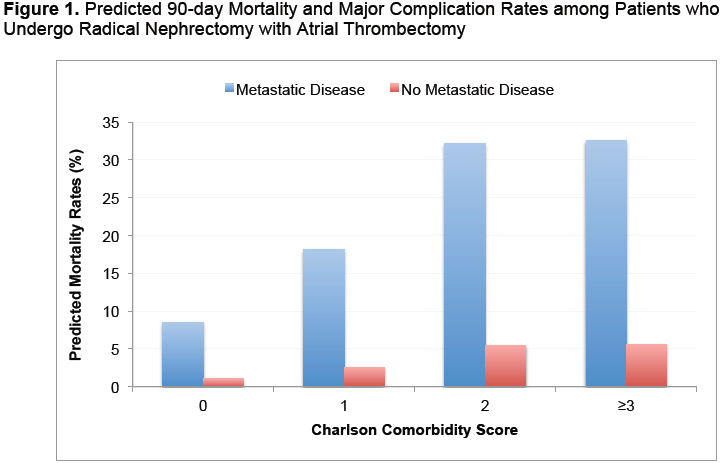
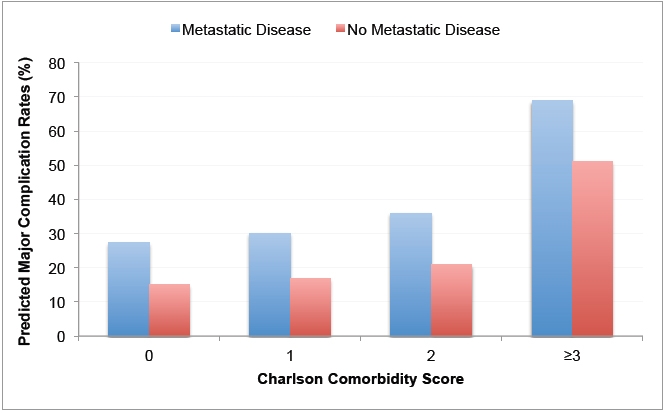
Our study cohort included a weighted sample size of 1176 patients; the majority were men (65.5%) and Caucasian (65.2%) with a mean age of 60.5 years. Over half (50.2%) of patients had metastatic disease while over one−quarter (26.1%) had significant comorbidities (i.e., Charlson Comorbidity Score (CCS) ≥2). Ninety−day major complication (Clavien grade 3−5) was present in 28.4% of patients with 10.1% suffering mortality (Clavien grade 5). On multivariable logistic regression, poorer Charlson comorbidity status was a significant predictor for both major complications and mortality, while having metastatic disease at the time of surgery was associated with 8.5-fold increased odds of mortality (OR: 8.5, p<0.01) (Table 1). Metastatic disease substantially increases the predicted probability of developing a 90-day major complication and mortality (Figure 1). Increased complication rate was not associated with age, gender, race, teaching institution, urban city, hospital size or region.
CONCLUSIONS:
We confirm that RN−AT is associated with significant morbidity and mortality. The mortality rate for this procedure exceeds those reported for other complex surgeries. The high morbidity and mortality among patients with metastatic disease stress the importance of appropriate pre-operative informed consent and consideration for alternate management paradigms including systemic therapy. Future studies are needed to compare the outcomes of RN−AT versus systemic therapy among patients with stage T3c RCC.
Back to 2014 Annual Meeting Abstracts
|

|

