|
|
 |
Back to Annual Meeting Program
Open versus Minimally Invasive Pediatric Pyeloplasty: A Contemporary Comparison of Cost in the United States
Briony K. Varda, MD1, Emilie Johnson, MD2, Curtis Clark, MD3, Benjamin Chung, MD4, Steven Chang, MD, MS1, Caleb Nelson, MD, MPH2.
1Brigham and Women's Hospital, Boston, MA, USA, 2Boston Children's Hospital, Boston, MA, USA, 3Pediatric and Adolescent Urology, Inc, Akron, OH, USA, 4Stanford School of Medicine, Palo Alto, CA, USA.
Introduction
Since the late 1990s, minimally invasive pyeloplasty has become an increasingly prevalent surgical approach for managing ureteropelvic junction obstruction in pediatric patients. Previous studies have suggested a possible cost equivalence and potentially cost savings for laparoscopic and robotic approaches, as compared with the open approach, due to decreased length of stay and reduced need for pain medications. The aim of our study was to compare the costs for open, laparoscopic, and robotic pyeloplasty in the United States.
Materials and Methods
We conducted a retrospective cohort study of pediatric patients (≤18 years) who underwent pyeloplasty (ICD-9 55.87) between January 1, 2003, and December 31, 2010. Our data source was the Premier Perspective database (Premier Inc, Charlotte, NC), which includes a nationally representative sample (20%) of US hospital discharges. We identified open, robotic and laparoscopic procedures through a review of hospital billing data. Descriptive statistics were used to characterize our study population. Bivariate and multivariate statistics were used to evaluate the relationship between surgical approach and perioperative outcomes of interest, including cost. Propensity score matching was used to adjust for selection bias, and survey weighting was used to yield a nationally representative result.
Results
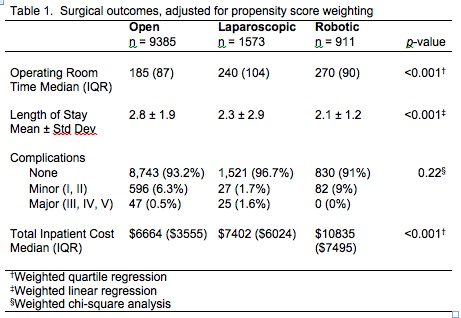
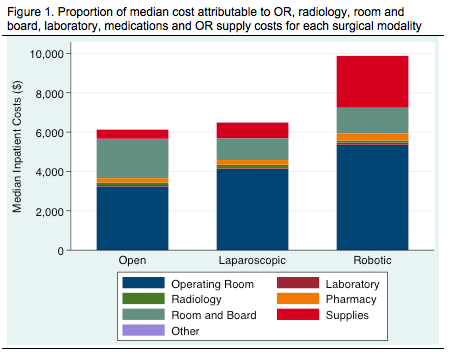
During the study period, the majority of pyeloplasty procedures were performed via the open approach (81%), in male patients (73%) who were Caucasian (69%), and in urban hospitals (96%). The incidence of complications was relatively low and similar among all three approaches (p=0.22). The mean length of stay was significantly higher for open (2.8 days) versus laparoscopic (2.3 days) and robotic (2.1 days) procedures (p<0.001) (Table 1). There was no difference in the mean pharmacologic costs (p=0.084). The median total inpatient costs were significantly lower among patients undergoing the open approach ($6,664) versus laparoscopic ($7,402) or robotic ($10,835) approaches (p<0.001), which is attributed to the higher operating room and supply costs for minimally invasive surgery (Figure 1).
Conclusion
Both robotic and laparoscopic pyeloplasty were significantly more costly than the open procedure despite shorter lengths of stays in the hospital. There was no reduction in the use of pharmacotherapy among patients undergoing minimally invasive pyeloplasty. The costs for operating room time and supplies for minimally invasive surgery, especially for robotic procedures, appeared to outweigh the cost savings associated with faster convalescence.
Back to Annual Meeting Program
|