|
Back to Annual Meeting Program
Medical Expulsive Therapy Utilization in Patients Presenting with Ureterolithiasis
Aaron Lay, MD1, Chen Feng, MD1, Benjamin Chung, MD2, Steven Chang, MD1.
1Harvard Medical School/Brigham & Women's Hospital, Boston, MA, USA, 2Stanford University, Palo Alto, CA, USA.
Introduction and objective:
Randomized controlled trials have demonstrated the efficacy of medical expulsive therapy (MET) for promoting passage of ureteral stones. Though this is well known among urologists, there has been concern regarding its utilization in the acute setting, when these patients may not be treated by urologists. We sought to measure utilization rates of MET in patients presenting with acute ureterolithiasis.
Methods:
We captured all patients who had a primary diagnosis of ureterolithiasis between January 1, 2003, and December 31, 2010, based on ICD-9 code 592.1 from Premier Perspective Database (Premier Inc, Charlotte, NC), a nationally representative discharge database that covers 20% of US hospital discharges. Patients who carried diagnosis of ureterolithiasis but did not undergo a surgical procedure were included in the study. Billing codes for tamsulosin, nifedipine, and predisone were collected. Statistical analyses were performed using STATA.
Results:
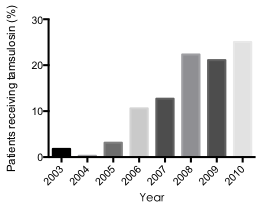
There were 2916 patients who had a principal diagnosis of ureterolithiasis but did not undergo a surgical procedure. Patients received tamsulosin 12.4% of the time, while nifedipine use was 1.5% and steroid use was 2.8%. Tamsulosin was more likely to be used in men, in teaching hospitals, and in recent years (Fig 1). Tamsulosin was more likely used in the Middle Atlantic States compared to other regions of the country.
Conclusion:
Even though there are randomized controlled trials that have demonstrated medical expulsive therapy to increase the likelihood of stone passage and faster time to stone passage, MET is underutilized. Our analysis suggests that MET is being used more frequently in recent years, but there is still underuse in the medical community.
Fig. 1
Back to Annual Meeting Program
|