|
|
 |
Back to Annual Meeting Program
Contemporary Trends in the Surgical Management of Renal Trauma in the United States
Julien Dagenais, MD1, Benjamin Chung, MD2, Steven Chang, MD1.
1Brigham and Women's Hospital, Boston, MA, USA, 2Stanford University Hospital, Stanford, CA, USA.
INTRODUCTION
Contemporary studies suggest that there has been a shift in the management of renal trauma with an increasing use of non-operative strategies as well as kidney surgery by non-urologists in some medical centers. To better define these trends throughout the United States, we performed a population-based assessment of practice patterns for the care of patients with renal trauma.
MATERIALS AND METHODS
Using the Premier Perspective database (Premier, Inc, Charlotte, NC), a nationally representative database capturing 20% of hospital discharges in the United States, we performed a retrospective study identifying all patients with renal trauma through the identification of International Classification of Disease, 9th Revision (ICD9) diagnosis codes (866.0x, 866.1x) between January 1, 2003, and December 31, 2010. Among the patients in the study cohort, we also identified those who underwent kidney surgical procedures with ICD9 procedure codes (55.x) as well as the specialty of the surgeon (urologist vs non-urologist) through review of the administrative data. We performed descriptive statistics as well as univariate and multivariate regression analyses adjusting for survey weighting.
RESULTS
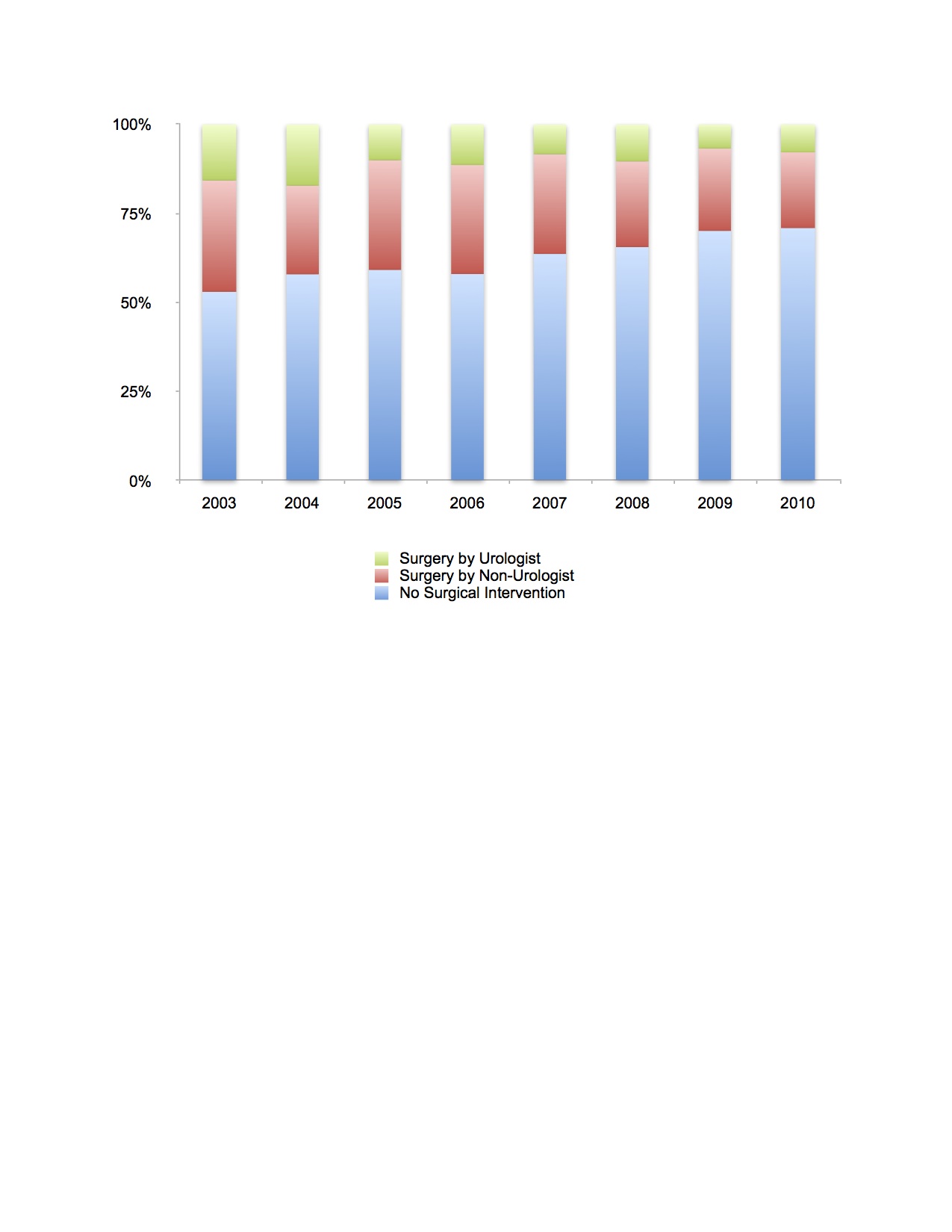
Our study cohort included a weighted sample size of 16,679 patients. During the study period, there was a statistically significant trend for non-operative management (OR 1.14, p<0.001) that increased from 53% in 2003 to 71% in 2010 (Figure 1). The yearly decrease in kidney surgery by urologists (OR 0.85, p<0.001) was more pronounced than for non-urologists (OR 0.91, p=0.004). Among patients undergoing kidney surgery, care by a urologist was associated with Caucasian patients (vs African-American, OR 2.78, p<0.001) and insurance coverage with Medicare (vs Managed care, OR 2.94, p=0.002). Hospital characteristics, including size (i.e., bed size), type (teaching vs non-teaching), and location (urban vs rural), were not related to the specialty of the surgeon performing kidney surgery. Urologists performed a larger number of complex reconstructive procedures (i.e., partial nephrectomy and pyeloplasty) compared with non-urologists.
CONCLUSIONS
A decreasing number of patients with renal trauma are undergoing operative management, a trend which reflects the growing knowledge that conservative treatment can be associated with favorable outcomes. Urologists, especially, are performing fewer surgical procedures for these patients, which may result in a decreasing number of complex, reconstructive kidney surgeries for patients with renal trauma. Understanding these practice patterns and clarifying their impact on clinical outcomes will be imperative for designing appropriate guidelines to manage renal trauma.
Back to Annual Meeting Program
|