|
|
 |
Back to Annual Meeting Program
Decreasing Suprapubic Tube Related Injuries - Risk Stratification and Recommendations for Percutaneous Suprapubic Tube Placement: Results of Case Series and Comprehensive Literature Review
Andrew J. Tompkins, M.D., Reed E. Watne, ScB, Michael Lasser, M.D.., Pamela Ellsworth, MD.
Brown University Alpert School of Medicine, Providence, RI, USA.
BACKGROUND:
Suprapubic tube placement (SPT) is a common urologic procedure with an unusually high mortality rate of up to 1.8% (Ahluwalia et al., 2006). Although infrequent, bowel perforation and obstruction are known complications of percutaneous SPT, occurring in approximately 0.3%-2.7% of cases (Sheriff et al., 1998; Cronin et al., 2011; Flock, Litvak, & McRoberts, 1978; Ahluwalia et al., 2006). As a result of 5 recent cases of bowel injury related to percutaneous SPT placement at our institution, we reviewed the literature in an effort to provide physicians with guidance regarding risk-stratifying patients for open as opposed to percutaneous SPT placement.
METHODS:
A literature review was performed with PubMed using the terms: suprapubic tube, bowel injury, and complication of suprapubic tube. Articles reporting percutaneous SPT placement related bowel injury were selected. Also, we reviewed 5 cases that recently occurred at our institution. Data from articles, including our 5 cases, was extracted to determine the technique of SPT placement utilized, underlying risk factors, and the nature of bowel injury.
RESULTS:
In addition to our 5 cases, 28 patients incurring bowel injury as a complication of percutaneous SPT placement were identified in a total of 18 papers or case reports. Two of the papers identified in the literature were excluded due to insufficient information (Sheriff et al., 1998; Ahluwalia et al.,
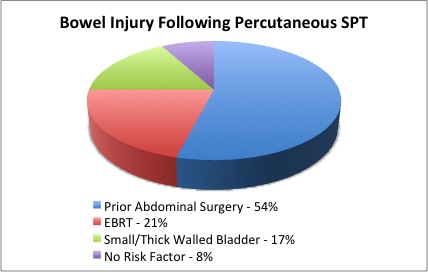
2006). Bowel injury complications presented both acutely after SPT placement (14/25, 56%) and later at the time of initial SPT change (11/25 44%). 92% of bowel injuries occurred in patients with clearly identifiable risk factors. Prior abdominal surgery (13/25, 54%), EBRT (6/25, 21%), and a small/thick walled non-distensible bladder (4/25, 17%) were common factors noted in patients with SPT associated bowel injury (Figure 1). Only 8% of bowel injuries occurred in patients without risk factors. Of these 24 patients, 3 had a Clavien class II complications, 20 had Clavien class IIIb complications, and 2 had a Clavien class V complications.
CONCLUSIONS:
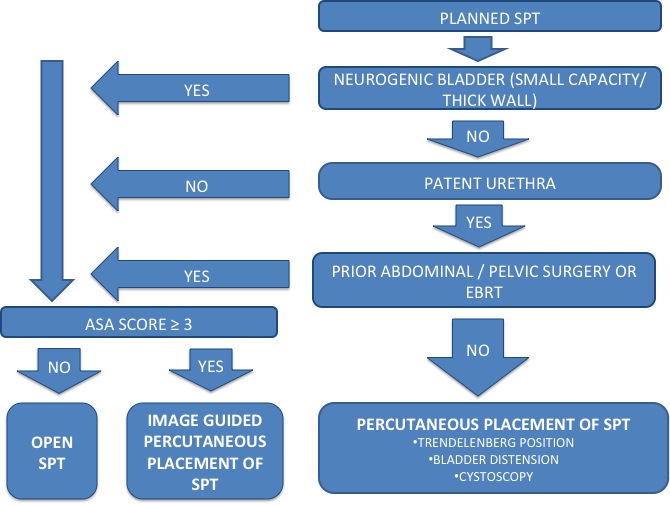
Prior abdominal surgery, abdominal/pelvic EBRT, and a small/thick walled non-distensible bladder are risk factors for percutaneous SPT associated bowel injury and are present in 92% of bowel injury cases. We advocate consideration of open or image guided percutaneous SPT placement in patients with small capacity or thick walled neurogenic bladders, those in whom the bladder cannot be distended adequately, prior abdominal/pelvic EBRT and/or surgery (Figure 2). If the patients ASA score ≥ 3, percutaneous image guided approaches should be used. If percutaneous SPT is planned, Trendelenburg positioning and the use of ultrasound and/or fluoroscopy at the time of SPT placement is supported by the literature review.
Back to Annual Meeting Program
|