|
Back to Annual Meeting Program
Pelvic Pain: Do Women with a Psychiatric Diagnosis Report More Pelvic Complaints?
Erik A. Pattison, MD1, Paholo G. Barboglio Romo, MD, MPH1, Veronica Triaca, MD2.
1Dartmouth-Hitchcock, Lebanon, NH, USA, 2Concord Urology, Concord, NH, USA.
INTRODUCTION: Female pelvic pain disorders are a heterogeneous group of diagnoses. A connection between such common psychiatric conditions as anxiety and depression with chronic pelvic pain has been reported in the literature. We report a retrospective review of women with the diagnosis of pelvic pain or dyspareunia. Our objective was to discern if such a connection existed in our cohort of patients.
METHODS: An IRB approved retrospective review of a cohort of 246 women with the diagnosis of pelvic pain or dyspareunia evaluated in a multidisciplinary Pelvic Medicine Clinic between January 2011 and November 2012. Self-reported validated questionnaires Pelvic Floor Distress Inventory (PFDI), the Pelvic Floor Impact Questionnaire (PFIQ) and each of their subcategories were analyzed. These surveys were answered in the waiting area before clinical visit without the interaction of any health care worker. Patients were then evaluated and pelvic pain and/or dyspareunia diagnosis were confirmed by a urologist and a gynecologist. History and physical, demographic, as well as questionnaires data was extracted from initial visit encounter from the patient’s chart. The rating of the pain was classified into severe or mild based on PFDI-20 question #20 (Usually experience pain or discomfort in the lower abdomen or genital area?). Score answers of No (0), not at all (1) or somewhat (2) were assigned as “mild pain”. Answers of moderately (3) and quite a bit (4) were graded as “severe pain”. Continuous data were analyzed using student’s t-test, categorical data (patient’s variables) via the Pearson Chi Square test, and questionnaire’s outcomes via the Wilcoxon test.
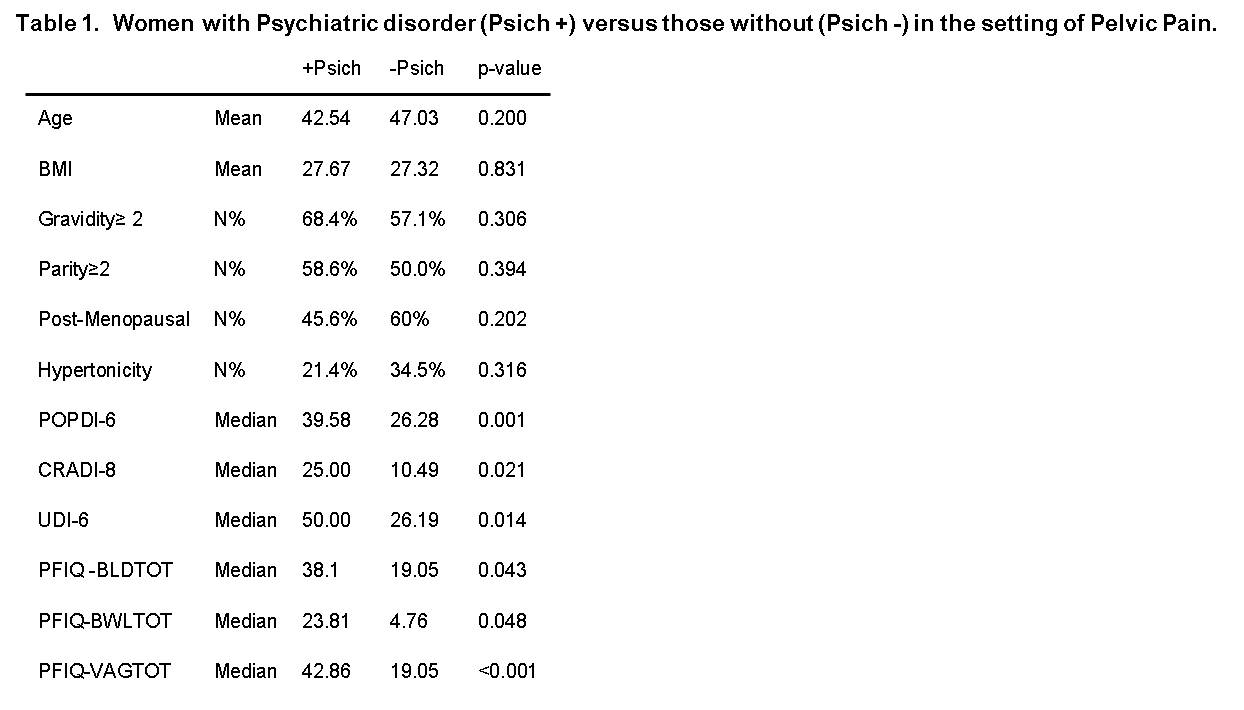
RESULTS: Pelvic Pain or dyspareunia was present in 246 patients and complete data was available for 89 women patients who met the criteria. Mean age was 44 years (SD+/-14.54). There was no significant difference between the groups with respect to age, BMI, pregnancy, menopause status, or the presence of pelvic hypertonicity on exam. Women with psychiatric comorbidity reported more pelvic symptoms in each instance; a significant difference was detected in both PFDI-20 (110 vs. 56, p<0.001) and PFIQ-7 (114 vs. 48, p=0.008) and in each of its subcategory questionnaires as displayed in Table 1. When assessing the severity of the pain, there were 44 with a higher degree of pain and 45 with a milder degree of pain based on item#20 of PFDI-20. Women with more severe pain had less (P<0.001) psychiatric comorbidities (15/44) when compared to those with a milder degree of pain (38/45).
CONCLUSIONS: Although our data suggests that women with severe pelvic pain have less psychiatric comorbidities, those with concomitant anxiety, depression or bipolar disorders report more overall pelvic complaints. These findings emphasize the potential for increased improvement outcomes in pelvic complaints with adequate treatment of psychiatric co-morbidity.
Back to Annual Meeting Program
|