|
Back to Annual Meeting Program
Effects of an intravesical nitric oxide donor on murine bladder function: Preliminary results
Saman Shafaat Talab, MD, Emmanuel S. Buys, PhD, Kenneth D. Bloch, MD, Warren M. Zapol, MD, Shahin Tabatabaei, MD.
Massachusetts General Hospital, Boston, MA, USA.
Effects of an intravesical nitric oxide donor on murine bladder function: Preliminary results
Saman Shafaat Talab1, Emmanuel E. Buys2,
Kenneth D. Bloch2, Warren M. Zapol2, Shahin Tabatabaei1
1Department of Urology, 2Department of Anesthesia, Anesthesia Center for Critical Care Research, Massachusetts General Hospital, Harvard Medical School, Boston, MA, USA
Background. Treatment of patients with cystitis in symptoms of an irritable bladder remains a clinical dilemma. Nitric oxide (NO) signaling plays an important role in urethral and bladder outlet function. However, the role of this inhibitory neurotransmitter on bladder muscle function remains unclear. Since the bladder is accessible for local pharmacotherapy, we examined the topical effects of an intravesically administered NO donor on murine bladder function in mouse and assessed any systemic side effects.
Methods. We studied anesthetized and mechanically ventilated female wild mice (C57BL/6, weighing 20-25 g). Bladder function was evaluated by measuring bladder pressure-volume (P-V) curves and continuous infusion cystometrographic (CMG) methods. In each mouse the bladder was infused at a constant rate (15 µL/min) with normal saline (control), and then sodium nitroprusside solutions (SNP, 1 mM or 0.1 mM) (for each n=4). In passive P-V curve studies, the bladder was exposed and a transurethral catheter was placed allowing infusions into the bladder and intravesical pressure monitoring. The bladder was mechanically inflated with either of solutions for 6 min followed by deflation of the bladder at the same rate and duration. In the active CMG study the bladder was continuously infused with similar solutions. The data from 6-10 consecutive active micturation cycles of each mouse was recorded for analysis. Mean arterial pressure and heart rate were monitored via a carotid arterial catheter throughout the studies.
Results. In passive bladder P-V curve studies, we observed considerable hysteresis, with deflation pressures considerably lower than inflation pressures. No significant difference between the 0.1 mM and 1 mM SNP group and the control group (saline) were noted. A continuous infusion of either SNP solution during active CMG studies did not alter measured cystometric parameters including the inter-micturation interval, the inter-micturation bladder pressure, the amplitude of bladder contractions, the duration of each contraction and the bladder compliance, when compared to the saline infusion. Intravesical infusion of 1 mM SNP decreased mean arterial pressure (-18.7%) and increased heart rate (+12.3%) (P<0.5), while infusion of 0.1 mM SNP solution infusion did not produce any systemic effects.
Conclusions. Infusing an NO donor into the bladder did not affect normal bladder smooth muscle tone. Although, normal bladder cystometric parameters were not affected with SNP solutions, 1mM infusion produced systemic hypotension and tachycardia. We found No effect on active cystometric parameters. These are preliminary results in an ongoing study. We plan to examine the effects of intravesical NO donor infusion in a murine model of cystitis. We hope to alter hyperactive bladder function in cystitis and cause minimal systemic side effects. 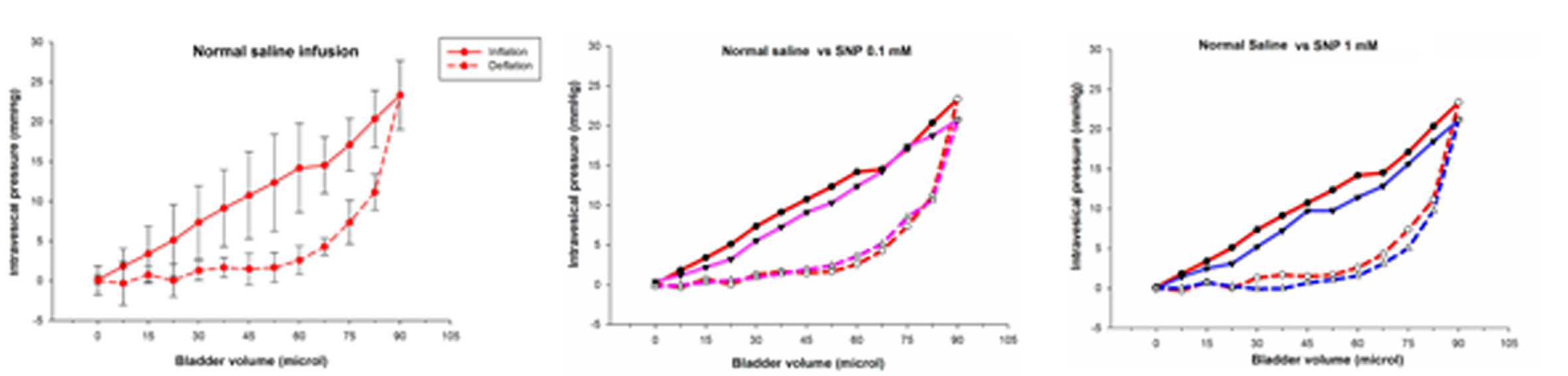
Back to Annual Meeting Program
|