|
|
 |
Back to Annual Meeting Program
Complications of Pelvic Lymph Node Dissection (PLND) during Robotic Assisted Laparoscopic Prostatectomy (RALP): A Single Institution Experience
Kristen R. Scarpato, MD1, Tyler Cottrell, BA2, Ilene Staff, PhD2, Alison Champagne, BS2, Joseph Tortora, MA2, Joseph R. Wagner, MD2, Stuart S. Kesler, MD2.
1University of Connecticut, Farmington, CT, USA, 2Hartford Hospital, Hartford, CT, USA.
INTRODUCTION
Pelvic lymph node dissection (PLND) at the time of robotic assisted laparoscopic prostatectomy (RALP) is commonly performed. While much uncertainty exists regarding the specific indications, optimum extent and survival benefit of nodal dissection, PLND is frequently performed during RALP with limited data regarding the potential additive complications. We compare rates of complications between two groups, those who underwent PLND and those who did not, at a single institution over six years.
METHODS
An IRB prospectively managed database was analyzed. 2191 patients who underwent RALP from January 2004 to December 2010 were included. Two groups were identified: Group One underwent RALP alone and Group Two underwent RALP with PLND. Patient age, Gleason score, clinical stage, estimated blood loss (EBL), length of hospital stay (LOS), positive margin rate and year of surgery were evaluated. All complications experienced were prospectively recorded, analyzed, and the fifteen most common are reported. Pearson Chi-square, Fisher's Exact, and Linear by Linear test statistics were used to determine statistical significance.
RESULTS
993 patients underwent RALP alone (Group One) while 1198 patients underwent RALP with PLND (Group Two). Rates of PLND per year reveal a trend towards more PLNDs over time. Patient age, pre-operative PSA, and EBL were found to be statistically different between groups. No difference in overall complication rate was found. Specific rates of complications that were found to be significantly higher in Group Two included delayed urine leak, incontinence, urinary tract infection (UTI), lymphocele and deep vein thrombosis (DVT).
CONCLUSION
Although the overall complication rate of those undergoing PLND during RALP was not statistically higher in our review, rates of major complications such as lymphocele and DVT were found to be significantly more common in patients after PLND. These additive risks should be considered during surgeon decision making and the consent process.
Table One: Patient and Operative Characteristics of Group One and Group Two
Table Two: Percentage of Specific Complications in Group One and Group Two 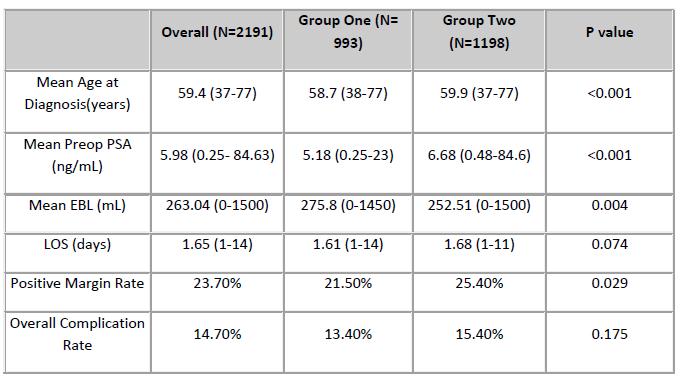 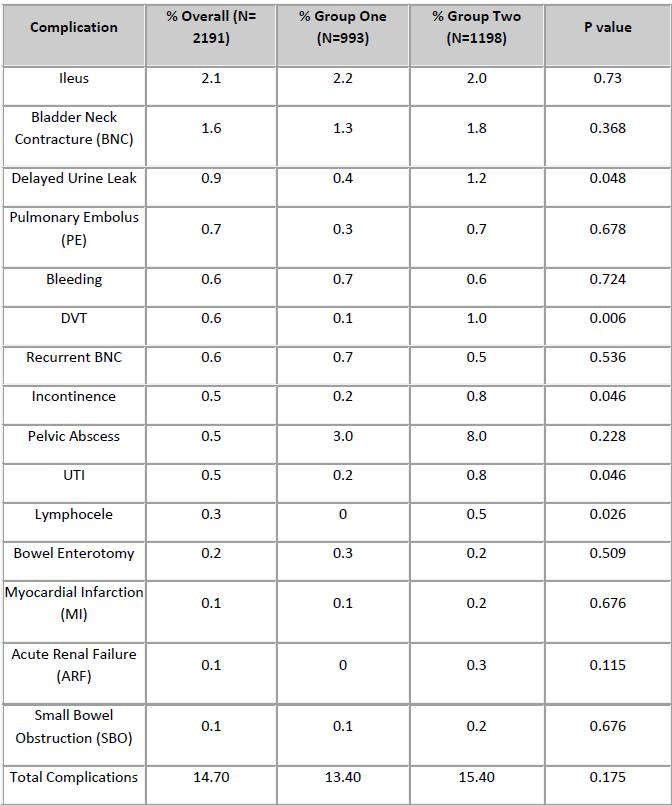
Back to Annual Meeting Program
|