|
Back to Annual Meeting Program
Radiofrequency Ablation Achieves Comparable Oncologic Control to Partial Nephrectomy for T1 Renal Cell Carcinoma in Poor Surgical Candidates
Sarah P. Psutka, MD, W. Scott McDougal, MD, Francis J. McGovern, MD, Peter Mueller, MD, Debra Gervais, MD, Adam S. Feldman, MD MPH.
Massachusetts General Hospital, Boston, MA, USA.
BACKGROUND: Radiofrequency ablation (RFA) of small renal masses (SRM) is increasingly offered to select patients with significant comorbidity as an alternative, less invasive, nephron-sparing therapy. Long-term comparisons of oncologic efficacy between RFA and partial nephrectomy (PN), the current gold standard for T1 renal cell carcinoma (RCC), are lacking. Our objective was to compare long-term oncologic outcomes between patients with clinical T1a and T1b RCC treated with either RFA or PN.
MATERIALS AND METHODS: We identified 551 patients who underwent nephron-sparing treatment for SRM between 1998 and 2008. Selection criteria for RFA included significant medical comorbidity and less than 10 year life expectancy. Exclusion criteria for this analysis included prior history of RCC, multiple synchronous tumors, metastatic disease at presentation, genetic predisposition to RCC, loss of follow-up prior to 6 months, or tumors other than RCC on biopsy or final pathology. A total of 380 patients fulfilled inclusion criteria, including 186 patients who underwent RFA and 194 patients who underwent PN (97 laparoscopically, 107 open). All patients undergoing RFA had biopsy-proven RCC. Primary endpoints included recurrence-free survival and overall survival.
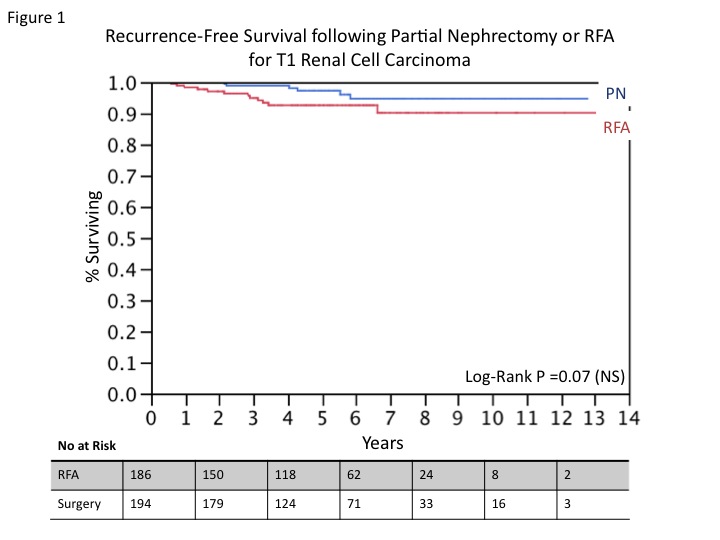
RESULTS: The mean (range) follow-up for RFA and PN were 4.8 years (0.5-13.1) and 5.4 years (0.5-12.8). Patients undergoing RFA were more likely to have larger tumors (3.1 vs. 2.6 cm, p<0.0001), be older (71.1 vs. 57.4 years, p<0.0001), and have a higher Charlson comorbidity score (5.6 vs. 3.5, p<0.0001). Of the patients undergoing PN, 17 had positive margins (8.8%) and 14 had pT3a disease (7.2%) on final pathology. There were 12 local recurrences (6.5%) in the RFA group compared to 6 (3.1%) in the PN group (p=0.12) with mean time to recurrence of 6.3 years vs. 2.7 years and similar recurrence-free survival (Figure 1, p=0.07). Overall mortality was higher in the RFA group (17.8% vs. 5.2%, p<0.0001), as was expected given the increased comorbidity and advanced age of patients in the RFA cohort. Death from RCC occurred in 4 patients treated by RFA and 1 treated with PN (p = 0.15).
CONCLUSIONS: Recurrence-specific survival and disease-specific mortality were comparable following RFA or PN for cT1a and cT1b RCC. For carefully selected patients with significant comorbidity precluding surgical intervention, RFA appears to provide durable oncological control for cT1 RCC in a nephron-sparing manner.
Back to Annual Meeting Program
|